Program At-A-Glance
Organizations: UPMC for Life Dual Health Plan and Community Care Behavioral Health Organization
Goal: Address fragmentation of physical and behavioral health services for dually eligible members with serious mental illness.
Key Elements: (1) Risk stratification to identify members with the most complex needs;
(2) in-depth training for care managers on physical and behavioral health services and recovery-based care models; and (3) intensive care management services.
Early Results: Reduced inpatient admissions for physical and behavioral causes, emergency department visits, and overall costs.
Nearly one-third of individuals who are dually eligible for Medicare and Medicaid have been diagnosed with a serious mental illness (SMI), such as schizophrenia, bipolar disorder, or major depressive disorder, a rate almost three times higher than for non-dually eligible Medicare beneficiaries.[i] Dually eligible beneficiaries with behavioral health conditions often must navigate different systems of care for their physical and behavioral health needs, as well as disparate systems of coverage under Medicare and Medicaid. Fragmented physical and behavioral health care, delivered across multiple providers and funding sources, can decrease access to care and lead to poor health status.[ii] In addition, mental health diagnoses drive spending in both Medicare and Medicaid for an already high-cost population; spending for individuals with a mental health disorder is more than twice that for dually eligible beneficiaries without such a diagnosis.[iii]
The UPMC Insurance Services Division is a provider-led organization that is part of an integrated health care delivery system affiliated with the University of Pittsburgh. It offers a range of commercial, Medicare, Medicaid, and behavioral health plans to more than 3.4 million members. UPMC’s Medicare Advantage Dual Eligible Special Needs Plan (D-SNP) — UPMC for Life Dual — was created in 2006 and nearly all of its 28,740 members reside in Pennsylvania. UPMC for Life Dual has a presence in most Pennsylvania counties and will be statewide in 2020. Approximately 47 percent of UPMC’s for Life Dual members are also enrolled in its Medicaid managed long-term services and supports (MLTSS) plan under Pennsylvania’s Community HealthChoices program.
PRIDE Case Study
This case study is part of a series made possible by The Commonwealth Fund through the Center for Health Care Strategies’ PRomoting Integrated Care for Dual Eligibles (PRIDE) project, a learning collaborative of nine leading health plans to advance promising approaches to integrating and enhancing Medicare and Medicaid services. Case studies highlight how plans participating in PRIDE are working with delivery system partners to advance innovative care management practices for dually eligible populations.
Forty percent of UPMC for Life Dual members have an SMI diagnosis. In 2017, UPMC for Life Dual launched a targeted care management program with Community Care Behavioral Health Organization (Community Care), a managed behavioral health organization that is also a UPMC company, to address fragmentation of physical and behavioral health services for its dually eligible members with SMI.[iv] This case study, made possible by The Commonwealth Fund, describes this robust care coordination and member engagement model that seeks to: (1) reduce emergent and unplanned inpatient admissions and (2) optimize health outcomes, quality of life, and self-management skills.
Impetus for the Program
In Pennsylvania, Medicaid behavioral health services are separately managed by county-based behavioral health managed care organizations. Community Care, one of these behavioral health organizations, is also part of the UPMC Insurance Services Division. It manages behavioral health services for most UPMC for Life Dual members in Allegheny County and offers several community-based programs focused on minimizing institutional care and maximizing family and community support and involvement. UPMC health plans and Community Care have a decade-long history of testing approaches to improving collaboration, accountability, and integration of physical and behavioral health care services for adult Medicaid beneficiaries with SMI and co-occurring physical health conditions.[v] The care management program that UPMC for Life Dual developed with Community Care is a natural extension of this relationship and will further both partners’ goals of improving coordination for beneficiaries with both Medicare and Medicaid coverage.
UPMC health plans and Community Care have a decade-long history of testing approaches to improving collaboration, accountability, and integration of physical and behavioral health care services for adult Medicaid beneficiaries with SMI and co-occurring physical health conditions.
As of June 2019, UPMC for Life Dual has over 8,500 members with SMI and substance use disorders who also have several chronic conditions such as heart disease, diabetes, asthma, and urinary tract infections that can lead to avoidable emergency department visits and inpatient admissions when not effectively treated. Unmanaged chronic conditions in individuals with SMI can also lead to lower life expectancy.[vi] To combat these trends and improve the management of physical health services, UPMC for Life Dual and Community Care developed a model in which care managers, who are embedded in community mental health centers, have in-person interactions with high-need members and provide additional telephonic support. Health plan leaders who designed this model focused on:
- Leveraging the existing partnership between UPMC for Life Dual and Community Care as two entities within the UPMC Insurance Services Division. Under this model, D-SNP enrollees can access the rich behavioral health benefits available to Medicaid members in Community Care. Both organizations have a system in place to share data on physical and mental health service utilization and diagnoses.
- Streamlining care management functions across programs. Both organizations sought to reduce duplication of care management services and increase flexibility to better target care management to meet individuals’ needs. Medicare care managers typically focus on chronic medical conditions, so UPMC and Community Care designated care managers from Community Care who have both a behavioral health background and knowledge of chronic conditions to provide care management for both the Medicare and Medicaid plans.
- Expanding programs with strong internal and beneficiary support. Staff from both UPMC for Life Dual and Community Care, as well as the county-based behavioral health system and local advocacy groups, recognized the need for a comprehensive care management model supporting holistic, integrated service delivery approaches and were committed to ongoing collaboration. This model maintained the same services available before program launch and clearly communicated that the new care management program was a value-add to existing services.
Key Program Elements
UPMC’s targeted care management program for dually eligible members with SMI was launched in July 2017. Key program elements include: (1) a risk stratification model to identify members with the most complex needs; (2) in-depth training for care managers on physical and behavioral health services and recovery-based care models; and (3) intensive care management services including assessments, wellness planning, and medication management.
Risk Stratification
The risk stratification model identifies the highest-risk members who would benefit most from face-to-face care management. To create the risk stratification model, UPMC for Life Dual reviewed a combination of claims and diagnostic data (e.g., inpatient admissions, number of prescriptions, spending on different services, etc.) from both organizations. The plan built a model that stratifies individuals into four risk groups, including those with: (1) the highest physical health (PH) and behavioral health (BH) needs; (2) high PH and lower/moderate BH needs; (3) high BH and lower/moderate PH needs; and (4) lower/moderate PH and BH needs. Individuals in the first group, those with the highest PH and BH needs, were prioritized for in-person care management.[vii]
UPMC for Life Dual notes that although the richness of the data available was valuable for building its risk model, it was still challenging to develop criteria to prioritize how to support members who have very complex profiles. The data indicated that many people had serious conditions and extensive needs, making it difficult to categorize the relative severity of members’ needs and design care plans to address members’ greatest needs first.
Training for Care Managers
UPMC for Life Dual and Community Care worked collaboratively to hire and train staff with competencies in both physical and behavioral health care. The most important qualities sought in hiring care managers for this program were: (1) experience working with individuals with SMI; and (2) an understanding of and experience with the landscape of medical providers as well as community-based resources in Western Pennsylvania. Given the rural nature of certain communities in this region, the hiring process took longer than anticipated because it was challenging to identify candidates who were familiar with resources across several, sparsely populated counties. In addition to having several years of clinical experience, it was important for both organizations that care managers were well steeped in recovery and service coordination care models.
Staff receive cross training to provide comprehensive care management for physical and behavioral health needs, including longitudinal care management, trauma-informed care, wellness plan development, and care coordination for chronic conditions across a continuum of severity. Care managers regularly meet in the field individually with supervisors and in small groups for ongoing support. The organizations also provide open access to both medical directors and psychiatrists for clinical consultation.
Intensive Care Management Services
After a member is identified through the risk stratification model to receive in-person, high-touch care management for this program, within a few weeks a care manager conducts an in-home assessment to thoroughly examine the medical and social factors that can support or hinder recovery. This assessment includes a medication review and reconciliation, in partnership with pharmacists who offer follow-up with providers to identify potential medication complications.[viii] Care managers then work closely with members to develop wellness plans, which identify members’ family and community supports as well as early warning signs for emerging issues.
Care managers may accompany members to appointments and screenings, either in-person or by phone. This in-person presence and direct participation helps care managers to identify and reduce gaps in care, and manage the closing of those gaps most effectively.
Program Goals and Impact
UPMC for Life Dual expects that this program will improve member and provider engagement and hopes to see resulting enhanced utilization patterns and improvement to its overall Medicare Advantage Star rating in the next 18 months.[ix] Its specific goals are to: (1) reduce emergency department visits and unplanned inpatient admissions; (2) optimize health outcomes through increases in preventive and wellness services and more timely, targeted interventions; (3) enhance and support quality of life and self-management skills; (4) increase member satisfaction; and (5) improve engagement in primary and specialty care, including behavioral health and substance use services.
The quality departments in both organizations work collaboratively to select quality metrics, and collect, and analyze data to identify opportunities to improve program design and member outcomes. Key metrics include:
- Clinical outcome measures, such as Healthcare Effectiveness Data and Information Set(HEDIS) all-cause readmissions, colorectal cancer screening, and medication adherence related to diabetes, hypertension, and cholesterol screening.[x]
- Social outcome measures, such as community tenure. UPMC for Life Dual examines community tenure — the amount of time individuals can remain in the community between inpatient admissions — as a key indicator to assess if robust care management services can help people avoid unnecessary admissions.
- Quality of life and member satisfaction with the program and services as assessed in member experience surveys.
- Process measures that assess care coordination and the extent to which care managers are closing gaps in care.
Both organizations have invested in data capacity and reporting. They use a care management information system that identifies various care manager-member touch points, including interactions with physicians, behavioral health providers, and community-based organizations. It also captures service needs, and how and when care managers make connections to fulfill them. For example, system markers flag potential gaps in care as claims are received, and care managers can use that data to target efforts to close existing gaps. The system generates reports to note when these gaps are closed.
In addition to the care management information system, UPMC developed reporting functions and data dashboards to reflect engagement activities, including accompanied provider visits, phone calls, face-to face meetings, and overall utilization. These reports stratify utilization and engagement data across the four risk categories to identify emerging patterns and adjust interventions. UPMC also analyzes this data to better understand how to target services to individuals with SMI to improve overall plan performance.
Initial Results
Preliminary analyses demonstrate a 10 percent downward trend in the 30-day readmissions rate for enrollees, while the rate of post-hospitalization follow-up within five days of discharge has an upward, positive trend.
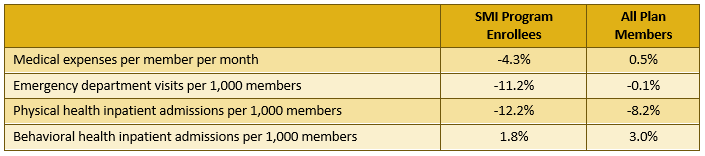
As of June 2019, UPMC has enrolled over 1,400 members with SMI in the program through completion of the initial in-home assessment. The program results to date show decreases in costs and acute care utilization measures for program participants. Total medical expenses for program participants decreased from year one (2017-2018) to year two (2018-2019), while total medical expenses for all UPMC for Life Dual plan members slightly increased. Program participants also experienced reductions from year one to year two in rates of emergency department visits as well as inpatient admissions for physical and behavioral health causes. Although UPMC for Life Dual decreased emergency department visit and inpatient admission rates for all members during this period, the rates for program participants decreased more than the rates for all plan members. Considering that individuals with SMI incur higher spending nationally, these findings are noteworthy. The full comparison of trends between program enrollees and all plan members are detailed in Exhibit 1.
Exhibit 1. Changes in Cost and Utilization for Program Enrollees as Compared to All UPMC for Life Dual Plan Members from Intervention Year 1 to Year 2
In addition, UPMC for Life Dual conducts the Quality of Life, Enjoyment and Satisfaction Questionnaire with program participants at enrollment and six months later.[xi] Of the 533 members who completed both surveys, more than half showed an increase in their second score. There were also improvements in questions assessing overall life satisfaction as well as satisfaction with medication.
UPMC continues to analyze available data to assess metrics on program outcomes and costs. Preliminary analyses demonstrate a 10 percent downward trend in the 30-day readmissions rate for program enrollees, while the rate of post-hospitalization follow-up within five days of discharge has an upward, positive trend. Data on clinical outcomes from HEDIS measures is not yet available for publication.
Insights
Both organizations are evaluating how to effectively target resources as members’ needs ebb and flow to ensure that those with the most severe needs receive the right care at the right time.
UPMC for Life Dual offers several lessons for other plans, providers, or states seeking to implement a care management model that attends to both the physical and behavioral health needs of dually eligible Medicare and Medicaid beneficiaries:
- Set clear goals. Be clear about initial goals and the timing of project milestones before program launch. Establishing well-defined parameters can improve troubleshooting and support future analyses to identify areas for program improvements. Examples of questions to address and adjust to a specific timeframe include: What is the overarching goal of the program? How should the overarching goal and interim milestones be measured? What result would achieve a significant improvement in quality?
- Identify data sources for risk stratification. Understand the best data sources and how that data can be used to identify different subsets of high-need populations. UPMC for Life Dual initially used Hierarchical Condition Category data, a risk adjustment model used by the Centers for Medicare & Medicaid Services to rank diagnoses into categories that represent conditions with similar cost patterns and to stratify members in different risk tiers. However, that data was more than one year old and did not capture members’ current clinical profiles. As a result, the plan decided to design its own risk stratification system using physical and mental health claims data.
- Prioritize interventions to maximize effectiveness. Balance care managers’ ability to improve care for individual members with achieving scale for the program. The entire population targeted for this program has very high needs. Plan leadership and care managers are learning how to set program priorities that attain meaningful improvements in individuals’ lives while stretching resources to serve a larger population. For example, they are working to better understand how to leverage supports from providers to complement care managers’ hands-on work and avoid duplication of efforts. Furthermore, care managers have to remain flexible with interventions. The plan found that members switched risk stratification tiers more frequently than expected. Both organizations are evaluating how to effectively target resources as members’ needs ebb and flow to ensure that those with the most severe needs receive the right care at the right time. They are also exploring how to better target resources for the population with “rising risk.”
- Tailor program design to the specific environment. The plan found that implementing an in-person care management program in rural counties creates additional challenges due to the time required to reach members across a large geographic area and the subsequent reduction in patients seen per day. Additionally, rural communities often offer fewer local resources on which care managers can draw to support care plans.
Conclusion and Next Steps
As of June 2019, the UPMC for Life Dual and Community Care program has served over 1,400 members, care manager positions are fully staffed, and there is promising data on health outcomes for its participants. UPMC for Life Dual and Community Care continue to refine data analytic capabilities. For example, UPMC and Community Care are focusing on the extent to which calculated risk scores and predictive modeling can reflect member experiences and utilization, and ways to use that data to better target interventions. They are also focused on improving and expanding dashboard capabilities to ensure that the data presented supports care managers’ ability to develop and adjust engagement strategies, as well as for plan leadership to make program changes as appropriate.
About the Center for Health Care Strategies
The Center for Health Care Strategies (CHCS) is a nonprofit policy center dedicated to improving the health of low-income Americans. It works with state and federal agencies, health plans, providers, and community-based organizations to develop innovative programs that better serve people with complex and high-cost health care needs.
[i] Congressional Budget Office. “Dual-Eligible Beneficiaries of Medicare and Medicaid: Characteristics, Health Care Spending, and Evolving Policies.” June 2013. Available at: https://www.cbo.gov/sites/default/files/113th-congress-2013-2014/reports/44308dualeligibles2.pdf. This report classified Medicare enrollees as having a mental illness if they had a diagnosis from the previous year of schizophrenia; major depressive, bipolar, and paranoid disorders; or other major psychiatric disorders.
[ii] Medicaid and CHIP Payment and Access Commission. “Integration of Behavioral and Physical Health Services in Medicaid.” March 2016. Available at: https://www.macpac.gov/wp-content/uploads/2016/03/Integration-of-Behavioral-and-Physical-Health-Services-in-Medicaid.pdf. Cited S.P Melek, D.T. Norris, and J. Paulus. Economic Impact of Integrated Medical-Behavioral Healthcare: Implications for Psychiatry. Milliman, Inc., and American
Psychiatric Association, 2014. Available at http://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Professional-Topics/
Integrated-Care/Milliman-Report-Economic-ImpactIntegrated-Implications-Psychiatry.pdf. Also cited Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders, and Board on Health Care Services. “Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series.” 2006. Available at: http://www.nap.edu/catalog/11470.html232. Also cited F. deGruy, “Mental Health Care in the Primary Care Setting.” In Primary Care: America’s Health in a New Era, edited by M.S. Donaldson, K.D. Yordy, K.N. Lohr, and N.A. Vanselow. 1996. Available at: http://www.nap.edu/read/5152/chapter/16.
[iii] R. Frank. “Mental Illness and a Duals Dilemma.” Journal of the American Society on Aging, 37, no. 2 (2013): 47-53.
[iv] Center for Health Care Strategies. PRIDE Plan Profiles: University of Pittsburgh Medical Center. August 2018. Available at: https://www.chcs.org/media/UPMC-PRIDE-Profile-081018.pdf.
[v].J. Kim, T. Higgins, A. Gerolamo, D. Esposito, and A. Hamblin. Early Lessons from Pennsylvania’s SMI Innovations Project for Integrating Physical and Behavioral Health in Medicaid. Mathematica Policy Research and Center for Health Care Strategies. May 2012. Available at: https://www.chcs.org/media/PA-RCP_Early_Lessons_Brief051412.pdf.
[vi] N.H. Liu, G.L. Daumit, T. Dua, R. Aquila, F. Charlson, P. Cuijpers, B. Druss, et al. “Excess Mortality in Persons with Severe Mental Disorders: A Multilevel Intervention Framework and Priorities for Clinical Practice, Policy and Research Agendas.” World Psychiatry, 16, no. 1 (2017): 30-40.
[vii] All members with behavioral health diagnoses, regardless of their risk strata, have access to telephonic care management as needed.
[viii] Medication reconciliation is also provided to program participants following discharge from an inpatient setting.
[ix] The Centers for Medicare & Medicaid Services (CMS) uses a five-star quality rating system to evaluate the performance of Medicare Advantage (MA) health plans. This Star Rating system enables beneficiaries, payers, and others to compare plans across multiple dimensions. For more information about Star Ratings, refer to: https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/PerformanceData.html
[x] The Healthcare Effectiveness Data and Information Set (HEDIS) is a widely used set of performance measures in the managed care industry, developed and maintained by the National Committee for Quality Assurance (NCQA). For additional details on HEDIS measure, refer to: https://www.ncqa.org/hedis/measures/.
[xi] The Quality of Life Enjoyment and Satisfaction Questionnaire is a self-report measure designed to assess the degree of enjoyment and satisfaction experienced in daily functioning. For additional information, refer to: J. Endicott, J. Nee, W. Harrison, and R. Blumenthal. “Quality of Life Enjoyment and Satisfaction Questionnaire: A New Measure.” Psychopharmacology Bulletin, 29, no. 2 (1993): 321-326.




