Takeaways
- Partnering with patients and community members of color to understand needs and preferences is an important step in improving health outcomes and advancing health equity.
- Health care organizations are at various stages of developing partnership approaches that create meaningful relationships with patients and communities.
- This brief outlines considerations for health care organizations to improve partnership relationships with patients of color to inform program and policy design.
Effective patient engagement is critical to improve the quality of health care. However, alleviating the mistrust that often exists between health care organizations and patients — bred by long-standing bias, stigma, and racist practices — requires a cultural shift where patients, particularly those of color, feel valued.1 Engaging patients in care delivery and design can help improve health outcomes, support health care transformation efforts, lower costs, and advance health equity goals.2 Patient and Family Advisory Councils, for example, provide a structure for patients to share their perspectives with health care teams on how to improve care.3 While health care organizations see the benefit of engaging with patients to inform patient-centered and equitable care, they are in various stages of understanding partnership approaches that create meaningful relationships with patients and communities.
What is Patient Engagement?
Patient engagement means “patients, families, their representatives, and health professionals working in active partnership at various levels across the health care system — direct care, organizational design and governance, and policy making — to improve health and health care.”4
The Center for Health Care Strategies, with support from the New York Health Foundation and in partnership with ATW Health Solutions,5 assisted seven New York-based health care organizations in piloting strategies for engaging patients of color to advance health equity (see Exhibit 1, below).6 Drawing on the pilot experiences, this brief outlines considerations for health care organizations in developing more robust patient engagement strategies.
Exhibit 1. Engaging Patients of Color to Advance Health Equity Learning Collaborative: Participants and Project Focus
| ORGANIZATION(S) | PROJECT FOCUS |
|---|---|
| BronxCare Health System/ Sickle Cell Thalassemia Patients Network | Understand social barriers that prevent families of children with chronic illness, including sickle cell anemia, from keeping their medical appointments. |
| Hudson Valley Care Coalition | Create a Member Advisory Council to improve Medicaid Health Home program engagement and support the development of the Coalition’s network training program for care managers. |
| John Oishei Children’s Hospital of Buffalo | Improve patient show rates for primary care medical appointments by five percent. |
| Mohawk Valley Health System | Leverage lessons from community vaccination campaigns to prevent heart disease among underserved and underrepresented populations. |
| New York University (NYU) College of Dentistry CariedAway Program | Increase the number of students who receive school-based dental care in New York City public schools, particularly Title 1 schools in the Bronx. |
| The New York Foundling | Partner with local community-based organizations to better understand community trends and tailor culturally competent behavioral health services for youth. |
| St. John’s Episcopal Hospital | Increase the number of patients who attend their first outpatient appointment following an acute psychiatric episode (i.e., hospital admission or emergency department visit). |
The following considerations, distilled from the experiences of the learning collaborative participants, can help guide health care organizations in building more effective relationships with the patients and communities they serve. These five lessons can be applied broadly across health care settings to better understand patients’ experiences, inform care delivery decisions, and address long-standing health disparities.
- Build trust with patient partners over time.
- Tailor outreach strategies to resonate with patient populations.
- Use trauma-informed approaches to strengthen relationships with patient partners.
- Collect and use data in partnership with patients.
- Approach patient engagement with humility and patience.

Many barriers exist for health care systems seeking to effectively engage patients more equitably to inform program design. It is not enough to just invite patients “to the table.” A variety of barriers to effective engagement contribute to mistrust. These include entrenched racism and discrimination, lack of infrastructure to sustain patient engagement, and the power imbalance that exists between large health care systems and patients, particularly low-income and patients of color and differing health priorities. For health care organizations looking to partner with patients, an explicit commitment to long-term relationship development is needed and must start with building trust.7
- Emphasize organizational commitment. Before launching patient and community partnership activities, time and commitment from leadership and staff is required. True collaboration means that health care staff at all levels value the expertise that patients bring. Health care leaders will need to authentically message, both internally and externally, that patient engagement activities are a critical element of their organization’s efforts to achieve health equity. Hudson Valley Care Coalition’s (HVCC) leaders worked in partnership with care managers and Medicaid health home members to address systemic injustices in the health care system by developing anti-racist training materials for staff.8 HVCC surveyed current health home members and conducted one-on-one follow-up interviews to better understand patient experiences, particularly patients of color. The survey and interviews helped inform activities for HVCC’s Member Advisory Committee, which is charged with advocating for change within the HVCC network. HVCC developed organization-wide staff training to help care managers understand the impact of systemic racism and trauma on patients and is testing strategies to help care managers navigate these issues in a culturally sensitive way. All levels of the organization, including the Executive Director, quality improvement and program staff, and care managers have been engaged throughout the process by setting the vision, coordinating data collection efforts, and identifying members for the Member Advisory Committee whose perspectives are included in training design and implementation.
Prominent messages via social media and other public forums can share a health care organization’s position on addressing inequities in care and health outcomes to staff and the community. Leadership at the John Oishei Children’s Hospital in Buffalo, for example, announced their participation in the Engaging Patients of Color to Advance Health Equity learning collaborative in a publicly posted monthly update,9 demonstrating to staff and patients the importance of better understanding the barriers to health care access for individuals they serve.
- Identify a trusted messenger. Establishing relationships with patients and communities can start with seeking partnership with trusted community figures, such as religious leaders, community organizers, staff from community-based organizations, as well as patients who are already engaged with health care systems, including through patient family advisory councils and patient ambassador programs. In upstate New York, Mohawk Valley Health System (MVHS) partners with church leaders to coordinate the Healthy Heart Church Tour, which are informational sessions held over breakfast at community churches about cardiovascular health and preventive care.10 MVHS staff partnered with the local NAACP chapter and church leaders to encourage congregants to participate in the breakfasts. Staff at MVHS recognize the power of collaborating with faith-based organizations to improve trust between community members and the health care system, and the importance ofhealth care organizations meeting the community in places that are comfortable to them. In addition to the Healthy Heart Church Tour, MVHS and the NAACP also held vaccination and health education events at community centers throughout the region, led by MVHS staff who are from the communities.11
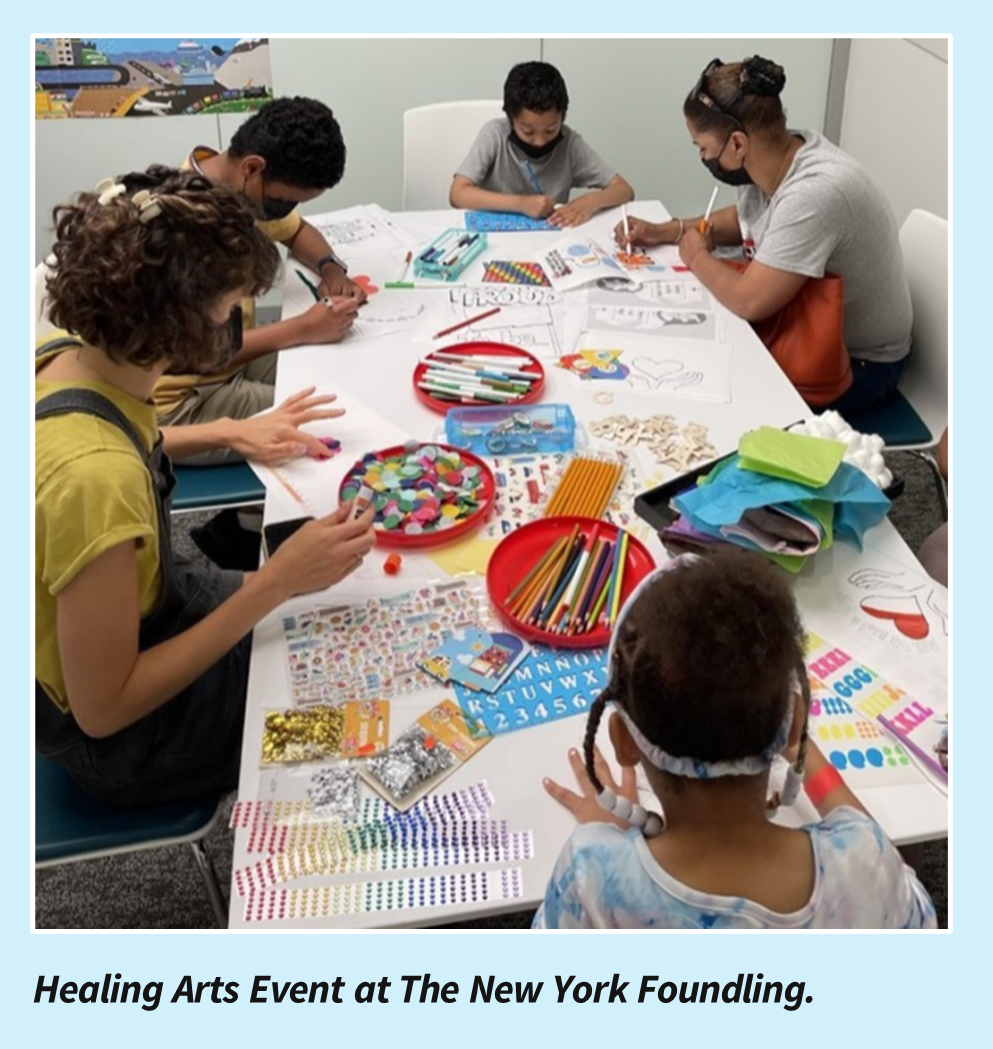
- Co-create a welcoming space. Another approach to building trust with patients is creating a safe and welcoming environment for community members within the clinical care space. Health care organizations can work with patients to better understand what this looks like and co-create engagement settings and activities that are driven by the preferences of patients in the community. This recognition of community member preferences signals a shift in power, which can help build trust and promote greater levels of engagement.12 The New York Foundling, for example, hosted a Healing Arts Event in its clinic to make the space feel less sterile and help patients and community members feel more welcome. To beautify the space, The Foundling created a community Art Sanctuary, which supported youth in creating artwork to hang throughout the clinic. Staff felt that the event helped to build connections with patients and plan to build on the Art Sanctuary by hosting a mural design and installation event, so that patients can see themselves on the clinic walls.
- Provide skill building opportunities and clear communication. To support meaningful patient engagement, health care organizations need to help staff and patients acquire the skills necessary to be effective partners as well as provide clear, ongoing communication. While some patients may be eager to partner with health care organizations, many may be unfamiliar with health care decision-making processes. As such, health care organizations can support community member participation by providing skill-building opportunities, including around public speaking, measures development, facilitation, budget development, and advocacy.13 These initial interactions with patients can forge the foundation for mutually beneficial relationships and ensure engagement activities are of value to both parties.
Health care organizations should also be transparent about patient engagement goals, decision-making processes, timelines, and expectations throughout engagement. To maintain trust, health care organizations should create formal processes for sharing progress and decisions with patients and community members.



Patients have diverse identities and lived experience, so there is not a “one-size fits all” approach to patient engagement. To build effective and equitable partnerships, health care organizations will want to tailor outreach strategies to effectively reach their populations of focus.
- Design engaging events. To improve their presence among communities being served, The New York Foundling, in partnership with the New York Council on Child and Adolescent Psychiatry, hosted a Hip-Hop Colloquium, a conversation about how hip-hop can be used to improve engagement with youth, particularly related to mental health and well-being.14 The virtual event focused on strategies to provide high-quality, culturally relevant mental health care to the increasingly diverse patient populations in the East Harlem area. The goals of the colloquium were to: (1) increase community interest and engagement in mental health; (2) increase student and trainee interest in mental health service delivery and psychiatry; and (3) provide a fun social event for New York City youth and families. The Foundling used social media to reach youth and involve them in planning the event. Gift cards were given to promote attendee engagement. The New York Foundling staff recognized that to build trust with community youth and grow their online presence, leveraging the expertise of young people was an important strategy.
- Foster connections with local champions. In communities where mistrust is often high between residents and the health care system, community champions are essential to help bridge the gap and foster partnerships. For the NYU College of Dentistry CariedAway Program, it was critical to effectively engage with parents of children in local schools and encourage them to sign the required consent form for their children to receive dental care in school settings. The program leaders identified “dental champions,” who serve as parent advocates for the school-based dental program and points of contact for students and their families. About 90 percent of the dental champions identify as people of color, bilingual, and reflect the school community.15 Children of parent advocates have used these dental care services and can share their experiences with other parents. The dental champions also support strategic development of the program, such as identifying barriers and solutions to increase the use of school-based dental services.

Incorporating the perspectives of patients and community members into health care practices is an essential step in developing an effective trauma-informed approach to care. Trauma results from events or circumstances experienced by an individual (i.e., physical, sexual or emotional abuse; adverse childhood experiences, including neglect and poverty; and discrimination and racism) that result in adverse effects on the individual’s functioning and well-being.16 A trauma-informed approach to care requires that health care organizations and care teams have a complete picture of a patient’s life in order to provide effective health care.17 To mitigate the impact of trauma, it is important for health care organizations to partner with patients to create a safe physical and emotional environment and co-develop screening and treatment processes to avoid re-traumatization.
- Integrate lived experience to make care more trauma-informed. Patients and community members can provide first-hand insights into how care is experienced and what changes an organization can make to improve quality and to reduce re-traumatization. For example, through its patient advisory council, St. John’s Episcopal Hospital learned that patients were severely traumatized receiving a needle injection using a restraint during emergency department visits, which contributed to individuals not returning for follow-up visits. Using a trauma-informed approach co-developed with the patient advisory council, the hospital implemented de-escalation training for staff and developed new protocols to avoid using restraints on patients and creating a safer, more welcoming environment.

Hospitals and clinics use data to guide improvement efforts, monitor progress toward goals, create accountability, and highlight successes. Data use includes clarifying how data will ultimately benefit patients through improved care; collecting and analyzing data; making sense of what those data mean; and taking action in response to what data show. It is important to engage patients in the collection and use of data to build trust and transparency, help stay focused on what matters most to patients’ health, and get a holistic view of what a care team is doing well and where to focus improvements efforts. Health care organizations can partner with patients in many ways in using data to better understand patient experience and make program improvements (See the tool, Steps for Engaging Patients and Community Members in Data-Driven Quality Improvement).
- Design data collection with patients. As noted above, engaging patients through all stages of data use is important, especially when designing a process to collect information. When response rates to patient surveys, interviews, or intake forms are low, this is often a sign that patients do not find the information collected meaningful, that the data collection process needs to be culturally appropriate, or that patients want to know more before sharing information. BronxCare Health System provided intensive training for social work interns to help them build relationships with patients and navigate complex discussions around social needs and missed appointments. For numerous reasons, such as mistrust and immigration fears, the BronxCare team was not able to collect as much information from patients as they had hoped, and the team recognized they need to more closely engage patients to understand how to initiate these sensitive conversations. In response, the team will explore building on the intern training sessions by integrating patient perspectives into the training modules and by having interns partner with patient mentors and “field-test” phones scripts with patients to ensure interns are approaching these conversations in a culturally supportive way.
- Listen to many sources of data. While health care organizations often think about data as something to be counted (quantitative) information also comes in the form of stories, text, and descriptions (qualitative). Several learning collaborative teams sought to establish formal mechanisms for collecting data from patients and communities, including through surveys and focus groups. Other teams were able to make program adjustments using data received through more informal mechanisms (i.e., intern and parent feedback). The NYU College of Dentistry CariedAway Program noticed that the rate of returned parent consent forms was lower than expected, and also received written feedback on consent forms, providing a clear message that the consent form was a barrier for some parents. The team is working on redesigning the consent form with parents to address their concerns and ultimately increase access to dental care in school settings.


Failure is often the first step toward success. It is important for individuals and organizations to approach this work with humility and patience, learn from mistakes, and make improvements to move toward more positive outcomes.
- Pivot as necessary. Patients often come to partnership opportunities with other life demands and stressors, lack of experience working in health care settings, and deep mistrust of health care organizations’ intentions and goals. It is important for health care organizations to have an open mind and adapt partnership approaches as necessary. For example, to better understand parent reluctance for their children to receive school-based dental care, staff from NYU’s CariedAway Program convened the Dental Champion Symposium to collect information on parent experiences, as well as school needs and expectations, and identify ways to reimagine the school dental care program. The symposium discussion revealed that each school uses a combination of different strategies to engage the parents and children participating in the dental care program. For example, one school communicates with parents and children through paper, email, telephone marketing, and school media platforms while another school uses personalized outreach to engage the community.
- Build a culturally sensitive environment. As health care organizations work to address health inequities and improve outcomes for patients, cultural humility and sensitivity are required. To improve vaccination rates among people of color and marginalized populations, the MVHS partnered with The Center, a community resource center for those who have recently immigrated to the community, to host vaccination clinics. The Center works with faith-based leaders to connect with refugees and about 75 percent of the staff represent the diverse ethnicities in the community. During one of the vaccine clinics, a woman requested to receive the immunization from a woman, especially since she was with her husband. The provider approached this with sensitivity and found a woman to administer the vaccine. While this was previously not on the radar for the health system, MVHS is now more mindful about cultural practices and has hired translators, is looking to expand cultural sensitivity training to additional providers, and continues to build connections with community leaders to improve care delivery for their diverse populations.
Incorporating lived experience and patients’ voices into decision-making processes is a critical element to ensure the equitable delivery of health care services. The most important component when fostering these partnerships is trust. While the approach to patient engagement may look different across health care systems and communities, it is a promising strategy to improve health outcomes and requires humility, patience, cultural sensitivity, and commitment from all levels of the organization. Patients value meaningful efforts by health care organizations to seek their perspectives and collaboration when designing and implementing programs and policies that directly impact their health and well-being and can help to advance health equity.
Endnotes
- L. Joszt. “5 Things About Medical Mistrust,” American Journal of Medical Care, August 2019. Available at: https://www.ajmc.com/view/5-things-about-medical-mistrust.
- S.H. Woolf, et al., “Authentic Engagement of Patients and Communities Can Transform Research, Practice, And Policy.” Health Affairs, 35(4), 590-594 (2016). Available at: https://www.healthaffairs.org/doi/epdf/10.1377/hlthaff.2015.1512.
- A. Spencer. Convening a Consumer Advisory Board: Key Considerations. Center for Health Care Strategies, December 2019. Available at: https://www.chcs.org/resource/best-practices-for-convening-a-community-advisory-board/.
- K.L. Carman, et al. “Patient and Family Engagement: A Framework for Understanding the Elements and Developing Interventions and Policies.” Health Affairs, 31, 2013. Available at: https://www.healthaffairs.org/doi/10.1377/hlthaff.2012.1133.
- To learn more about ATW Health Solutions, visit https://atwhealth.com/.
- To learn about CHCS learning collaborative, Engaging Patients of Color to Advance Health Equity, visit https://www.chcs.org/project/engaging-patients-of-color-to-advance-health-equity-a-learning-collaborative/.
- A. Spencer and A. Nuamah. Building Effective Health System-Community Partnerships: Lessons from the Field, Center for Health Care Strategies, March 2021. Available at: https://www.chcs.org/media/Community-Partnership-Pilot-Brief_3.2.21.pdf.
- New York Department of Health. Medicaid Health Homes – Comprehensive Care Management. Available at: https://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/.
- Progress, But Challenges Lie Ahead, An Update from Bob Nesselbush, CEO of Kaleida Health. August 2021. Available at: https://www.ochbuffalo.org/news/read/An-Update-from-Bob-Nesselbush-CEO-of-Kaleida-Health/16862/.
- Rome Daily Sentinel. NAACP, MVHS and Churches Partner on Heart Health Sessions, April 2022. Available at: https://romesentinel.com/stories/naacp-mvhs-and-churches-partner-on-heart-health-sessions,133092.
- A. Ohene-Ntow and A. Spencer. Healthy Heart Church Tour: A Unique Community Partnership to Advance Racial and Health Equity Center for Health Care Strategies, July 2022. Available at: https://www.chcs.org/healthy-heart-church-tour-a-unique-community-partnership-to-advance-racial-and-health-equity/.
- NORC at the University of Chicago: MCO Learning Hub. Spotlight on Member Engagement and Elevating the Consumer Voices: Commonwealth Care Alliance (CCA) and the Center to Advance Consumer Partnership (CACP). April 2021, Available at: https://www.norc.org/PDFs/Medicaid%20Managed%20Care%20Organization%20Learning%20Hub/MMCOLearningHub_CCA.PDF.
- A. Spencer and A. Nuamah. Building Effective Health System-Community Partnerships: Lessons from the Field, Center for Health Care Strategies, March 2021 https://www.chcs.org/media/Community-Partnership-Pilot-Brief_3.2.21.pdf.
- The New York Foundling, Learning to Walk Without Feet, A Colloquium of Hip-Hop, Healing and Resilience. Available at: https://www.nyfoundling.org/event/learning-to-walk-without-feet-a-colloquium-on-hip-hop-healing-resilience/.
- NYU College of Dentistry, CariedAway Program. Application. 2021.
- Center for Health Care Strategies, 10 Key Ingredients for Trauma Informed Care. Available at: https://www.traumainformedcare.chcs.org/wp-content/uploads/2018/11/Infographic-TIC.pdf.
- Center for Health Care Strategies. What is Trauma Informed Care? Available at: https://www.traumainformedcare.chcs.org/what-is-trauma-informed-care/.




