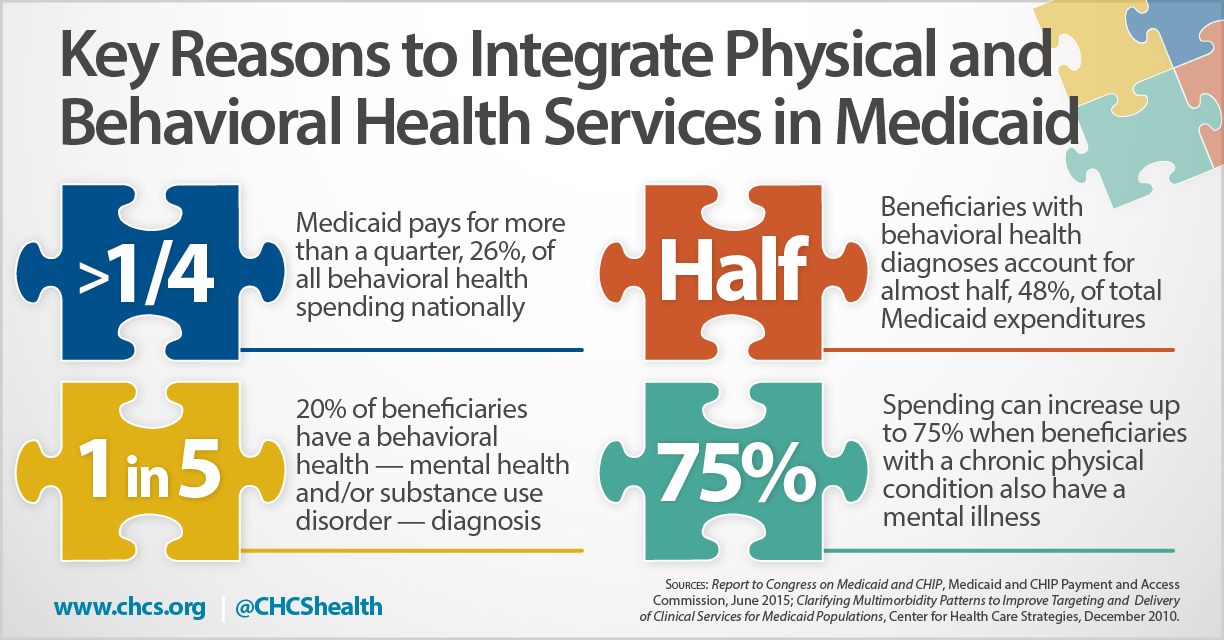
A significant number of Medicaid beneficiaries — one in five — have a behavioral health diagnosis (mental health and/or substance use disorder). However, many of these individuals are served in fragmented systems of care with little to no coordination across providers, often resulting in poor health care quality and high costs.
This infographic from the Center for Health Care Strategies (CHCS) spotlights four key data points that help build the case for integrating physical and behavioral health services in Medicaid. See also a related CHCS brief, Integrating Behavioral Health into Medicaid Managed Care: Design and Implementation Lessons from State Innovators, that explores how five innovator states have integrated behavioral health within managed care arrangements.