Many states across the country are seeking to dramatically improve health care quality, contain costs, and maximize the value of health care investments, particularly for Medicaid populations. One major opportunity to further such efforts, the Delivery System Reform Incentive Payment (DSRIP) program, is garnering growing attention among state and federal policymakers. Unlike other delivery system reform activities targeted to primary care providers and medical groups, DSRIP is anchored in hospital system-based improvement efforts. As such, DSRIP can serve as a provider-based building block for other broader, multi-payer health care transformation efforts, including the State Innovation Models.
Authorized through Medicaid Section 1115 waivers, DSRIP allows states to reward eligible hospitals for meeting performance milestones on defined care delivery improvements. DSRIP is financed by redirecting disproportionate share hospital (DSH) payments traditionally used by public hospitals for the provision of uncompensated care. To qualify for federal matching, state waivers must meet budget neutrality requirements and generate “savings” (i.e., reduce the federal cost of operating Medicaid) that can be reinvested with matching state funds in delivery system reform activities.
DSRIP programs generally address four key domains, with increasing focus on outcomes over the course of implementation:
- Infrastructure development;
- System redesign;
- Clinical outcomes improvements; and
- Population-focused improvements.
State DSRIP Status Update
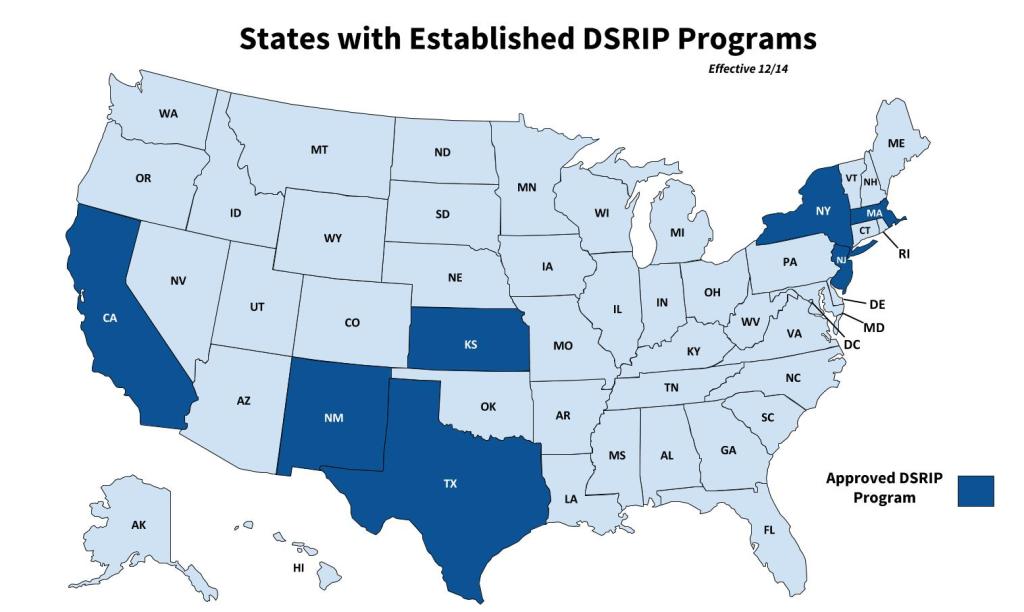 Since 2010, seven states have established DSRIP programs, including California, Kansas, Massachusetts, New Jersey, New Mexico, New York, and Texas, with several others expressing interest.
Since 2010, seven states have established DSRIP programs, including California, Kansas, Massachusetts, New Jersey, New Mexico, New York, and Texas, with several others expressing interest.
DSRIP approaches have evolved considerably over the past few years. Some of the first DSRIP programs were focused on reallocating funding to safety net hospitals only. More recent models in New York and Texas have advanced wider-scale payment and delivery system reform by expanding the definition of eligible safety net providers to encourage community-wide collaboration. States are now partnering with providers and payers to design and implement more standardized outcomes-oriented improvement projects with defined metrics and reporting requirements. Beyond these general trends though, each state’s DSRIP program has unique features tailored to the state’s hospital systems and Medicaid transformation context.
New York’s Medicaid Transformation via DSRIP
New York is the latest state to launch a DSRIP program. Its comprehensive initiative, approved in 2014, includes a broad set of providers and range of improvement projects. The state’s primary goal under DSRIP is to reduce avoidable hospital use by 25 percent. Under New York’s definition, avoidable hospital use encompasses preventable hospital readmissions as well as inpatient admissions that can be avoided with proper preventive care services. New York’s DSRIP program, designed to change care for both Medicaid beneficiaries and uninsured New Yorkers, will run for five years beginning in April 2015.
The state’s DSRIP program will hold comprehensive networks of providers jointly accountable as Performing Provider Systems (PPS) for delivering population-based health care. The program is open to hospital and non-hospital based providers, which must meet specific eligibility criteria to share in performance payments. Funding for this work stems from New York’s recent Medicaid Redesign Team (MRT) waiver amendment that allows the state to reinvest $8 billion of the $17.1 billion in federal savings generated by MRT reforms, more than $6 billion of which has been allocated to support the state’s DSRIP program.
California: Revamping DSRIP to Drive Accountability
As part of its “Bridge to Reform” Waiver renewal in early 2015, California is looking to build on the achievements and lessons from its 2010 DSRIP efforts as well as other states’ experiences. California’s current DSRIP program rewards 21 safety net hospitals with more than $3.4 billion for achieving quality benchmarks associated with specific projects. Under its renewal efforts, the state is gathering input from a wide range of stakeholders to place greater emphasis on meeting outcomes-based quality benchmarks and achieving greater consistency across the safety net system. Key areas of interest include patient safety, complex patients, and prevention. The state is also exploring how it might use DSRIP to: (a) advance the integration of behavioral health and substance use disorder services with medical care; (b) promote care coordination across delivery systems; and (c) potentially include a broader set of safety net providers.
Learn more
The experiences of states like California and New York can inform other state DSRIP design and implementation efforts. Learning how existing programs are defining provider eligibility, project components, and metrics can be helpful for states at the DSRIP starting block. This December 2014 CHCS webinar, New York’s DSRIP Program: A Model for Reforming the Medicaid Delivery System, provided a behind-the-scenes look at New York’s DSRIP design and implementation plans.




