Within publicly financed health care, there is a growing consensus that cross-sector collaboration is a necessary ingredient for improving beneficiary outcomes and reducing costs. This is driven by the recognition that there is a subset of individuals who touch multiple public systems — including Medicaid, food assistance, homelessness, housing supports, criminal justice, etc. — and whose outcomes and costs may be affected by involvement across these domains. Any care manager working with a Medicaid population could provide anecdotal evidence, but to date there have been few, if any, large-scale analyses examining the utilization of this population across multiple public sectors to provide a solid evidence base for cross-sector involvement.
To begin building a quantitative case for this idea, Minnesota’s Hennepin County Center of Innovation and Excellence, in partnership with the Center for Health Care Strategies and with support from Kaiser Permanente Community Benefit, recently measured cross-sector involvement among Hennepin County’s Medicaid expansion population and the way in which enrollees interact with several other county agencies and services. The results shed light on a high-need population that touches numerous public systems and reveals important insights into potential drivers for cross-sector utilization. The findings showcase why greater alignment across such sectors is needed, and highlights areas in which such collaboration may present significant opportunities to improve the quality of care for individuals with complex medical and social needs and reduce their overall costs to local, state, and federal governments.
Removing Barriers for Accessing Cross-Agency Data
One of the major barriers to studying cross-sector utilization is the difficulty in linking datasets from multiple agencies. Hennepin County is uniquely positioned to address this issue due in large part to its ongoing efforts to integrate health and social services. Over the past decade, the county has taken several steps toward creating a “totally” accountable care organization that goes beyond medical services to serve the “total” needs of patients. Hennepin Health, the county’s accountable care organization, serves Medicaid beneficiaries and comprises a major safety net hospital, the county-led Medicaid managed care plan, a federally qualified health center, and the county’s Human Services and Public Health Department (HSPHD). Created in 2006, HSPHD houses a variety of services that had previously existed in disparate departments, including health care programs, food and cash support, case management, and public health.
Both HSPHD and Hennepin Health have consistently collaborated with other sectors such as housing and criminal justice to more holistically address the needs of residents. This recent analysis was facilitated by the county’s data integration efforts, and by the fact that the state of Minnesota adopted a “single identifier” approach across several human services domains, meaning that identifiers can be linked across multiple data systems.
Cross-Sector Findings
The study examined a cohort of Hennepin County Medicaid enrollees who were enrolled in the program for at least one month between March 2011 and December 2014. Administrative data from the health care, human services, criminal justice, and housing (including emergency shelter and supportive housing) sectors were analyzed (Exhibit 1).
Exhibit 1: Public Sector Services Analyzed in Hennepin County
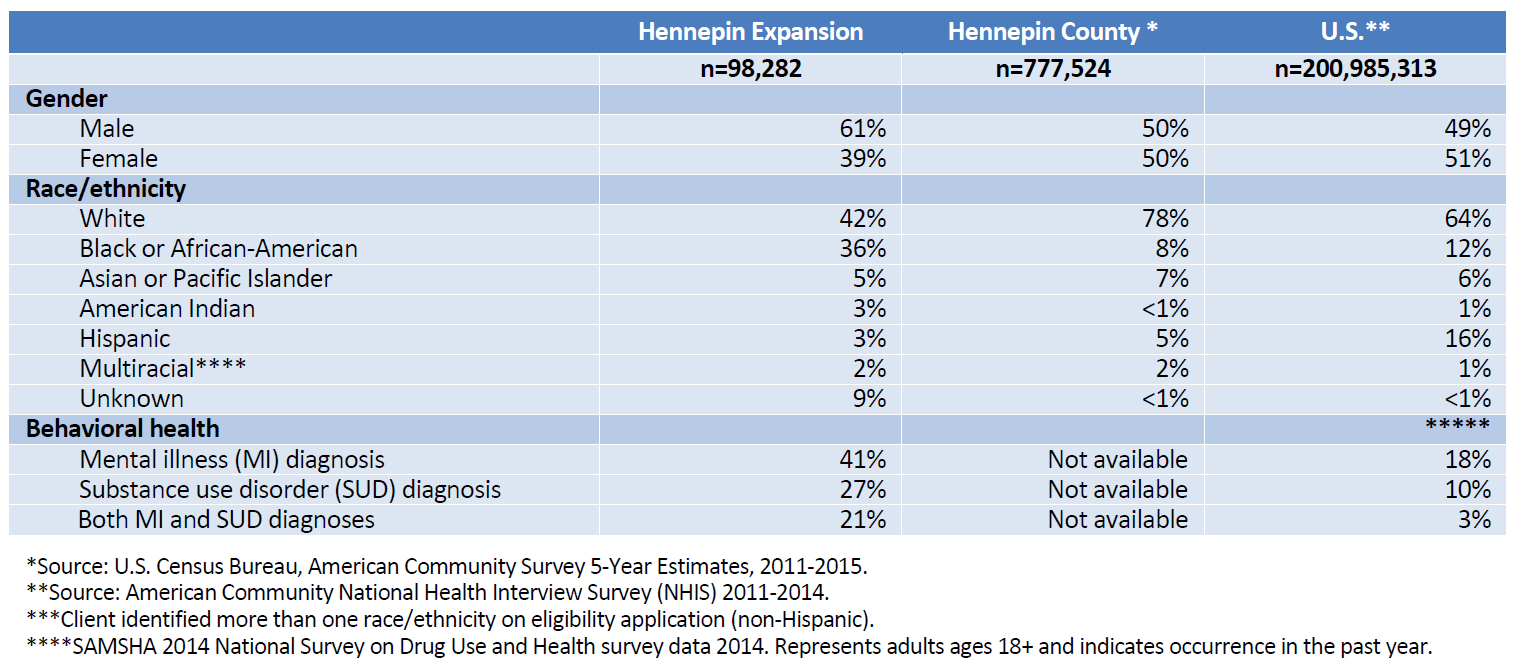
At a base level, the analysis provides a useful portrait of Hennepin’s Medicaid enrollees: they were disproportionately men (61 percent), English-speaking (89 percent), single (90 percent), Black/African-American (36 percent), and relatively young. A critical finding was that 41 percent of the population had a mental health diagnosis, 27 percent had a diagnosed substance use disorder, and 21 percent had both diagnosed mental health and substance use disorders. These rates are significantly higher than the national average (Exhibit 2).
Exhibit 2. Demographics of Hennepin Expansion Enrollees Compared to County and National Populations (Age 21-64)
Among the study’s many results, several are particularly useful for understanding the cross-sector utilization of this cohort:
- 93 percent of enrollees had contact with at least one sector over 46 months. Of these,
- 21 percent only used health care;
- 30 percent were involved in both health care and human services;
- 19 percent were involved in health care, human services, and criminal justice; and
- Eight percent were involved in all four sectors — health care, human services, criminal justice, and housing.
- Medicaid is a major source of health insurance coverage for residents who use other publicly funded services.
- While the Medicaid expansion population represented only 13 percent of the county’s population, 43 percent of individuals who used the county’s emergency shelters, 29 percent in the Adult Detention Center, and 48 percent in the Adult Corrections Facility were expansion enrollees at one time or another.
- Medicaid enrollees accounted for nearly 60 percent of all bed days in the county’s emergency shelter and over half of bed days in the criminal justice system.
- More than $600 million dollars were spent annually in the public sector on Medicaid expansion enrollees. Of this, over half was spent on health care programs ($344 million). The next highest cost sector was human services ($113 million), followed by criminal justice ($105 million), and then housing ($49 million).
- The spend was not allocated equally across all levels of government — federal and state government spent most on health care whereas county government spent most on criminal justice.
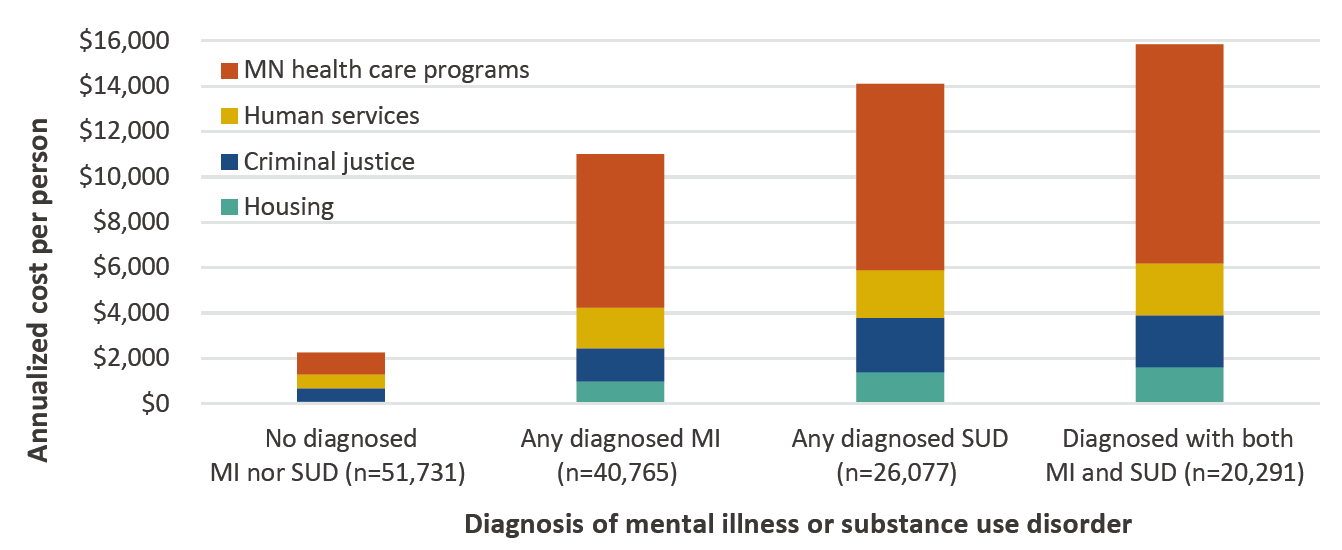
- Individuals with mental health and/or substance use disorder diagnoses disproportionately drove public sector costs. While only 21 percent of the expansion population, these individuals incurred 53 percent of all public costs (Exhibit 3).
Exhibit 3. Annualized Per Person Costs for Hennepin Expansion Enrollees with Substance Use Disorder or Mental Illness Diagnosis
Implications
This analysis makes clear that many Medicaid expansion enrollees used multiple public services beyond health care, particularly those with mental health or substance use disorder diagnoses, and accounted for a substantial proportion of public service use across sectors. The findings point to several recommendations for a more collaborative care delivery approach, including:
- Develop a more integrated approach to service delivery across sectors. Achieving comprehensive cross-sector coordination may be an important key for improving patient outcomes and reducing costs. For example, the data in this analysis highlight that enrollees with unstable housing and behavioral health conditions account for a large share of multi-sector involvement across sectors. Given this, collaborative efforts to integrate housing stability efforts with behavioral health treatment could result in positive effects across multiple sectors.
- Increase opportunities for integrating cross-sector data systems. Focusing on this aspect of the work will not only provide a baseline understanding of how individuals move through systems, but can also guide intervention design and support evaluations to ensure that effective strategies are being deployed. Gaining a fuller picture of cross-system utilization will also undoubtedly shed more light on the ways in which social determinants impact health (and vice versa) and highlight additional areas in which greater alignment may result in improved patient outcomes and financial savings across sectors.
- Establish a unified vision for public services. By and large, health care, human services, criminal justice, and housing systems at state, local and federal levels have developed their own approaches to service delivery and evaluation, including utilizing their own assessment tools and measuring distinct outcome metrics. This is in spite of the fact that many of these sectors are similarly impacted by social determinants and, as the Hennepin analysis shows, share clients. Developing a unified vision at the local and state levels that includes a shared framework for success, shared assessments, and outcome metrics is a critical component of achieving greater cross-sector collaboration and alignment. In addition, policymakers must consider how to align funding across sectors — Hennepin Health’s shared savings model is an example of how this can be achieved.
Hennepin Health has long championed the importance of cross-sector collaboration. Their pioneering efforts to integrate health care and social services and to develop payment structures to encourage such cross-sector collaboration are supported by this study. Further, this analysis adds an important evidence base to this argument, and highlights the potential of improved alignment.





The Colorado Health Institute just finished a similar study – not quite as in depth for the Mile High Health Alliance here in the city and county of Denver. You can find the report – “Follow the Money: Health Related Spending in Denver” here: http://milehighhealthalliance.org/wp-content/uploads/2017/08/Follow-the-Money-paper-v2.pdf
We’re contemplating next steps with the information, but clearly “we’re doing it wrong” based on the BMJ report on “Health and Social Service Expenditures: association with health outcomes” (Bradley, et alia), which looks at health outcomes in relationships to amount spent on medical versus social services in developed OECD countries. http://milehighhealthalliance.org/wp-content/uploads/2017/08/Follow-the-Money-paper-v2.pdf