COVID-19 has hit some populations harder than others. This includes people of color, residents of nursing facilities and other congregate settings, and individuals with multiple chronic medical conditions. People in these groups are often dually eligible for Medicare and Medicaid because they have a disability or are age 65 or older, and also have low incomes. Recent federal data show that dually eligible individuals are more likely to contract COVID-19 than Medicare-only beneficiaries and are hospitalized with COVID-19-related complications more than four times as often.
Dually eligible individuals also frequently have significant social risk factors, which if addressed, could improve their access to care, health outcomes, and quality of life. With support from Arnold Ventures, the Center for Health Care Strategies recently partnered with the Association for Community Affiliated Plans (ACAP) to examine how its Dual Eligible Special Needs Plan (D-SNP) members were addressing their enrollees’ social risk factors.
As a supplement to this work, ACAP and CHCS explored how ACAP-member plans, including D-SNPs and Medicare-Medicaid Plans (MMPs), are addressing existing and new social risk factors of their dually eligible enrollees during the pandemic. Information from 14 plans was collected in an October 2020 survey. This blog shares the survey results.
COVID-19 Exacerbated Existing Needs and Created New Challenges
Plans reported that prior to the pandemic, their enrollees’ greatest social risk factors were housing instability/homelessness, food insecurity, and lack of transportation. They began to see the impacts of COVID-19 on their dually eligible enrollees starting in March and April 2020. Most plans reported changes in enrollees’ needs related to social risk factors because of the pandemic, and they ranked where they saw the largest increases (see figure below). Food and social isolation/loneliness were the areas of greatest need, followed by housing, basic supplies (toilet paper, cleaning supplies), and personal protective equipment (PPE). Lesser, but still significant needs were reported around medical and non-medical transportation, domestic safety, and legal services (eviction/foreclosure).
COVID-19’s Effects on Enrollee Social Needs as Ranked by 14 ACAP D-SNPs
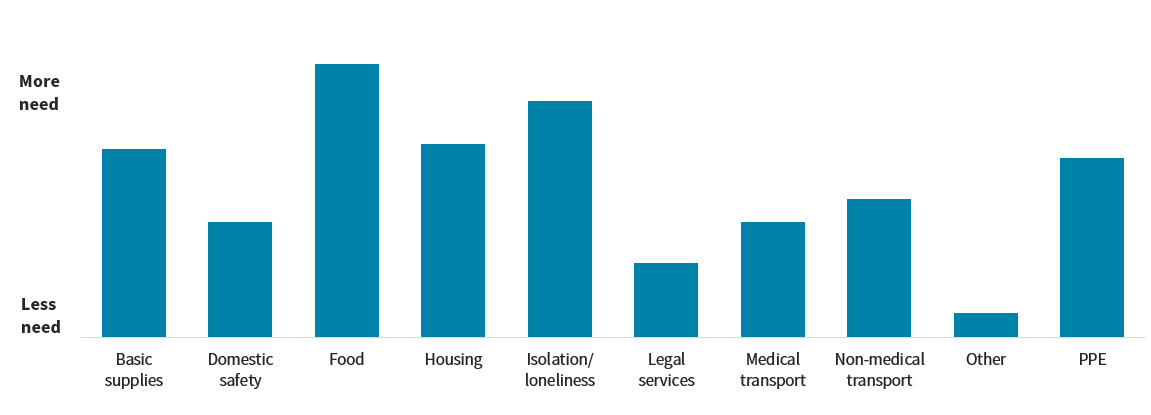
Categories of Enrollee Social Needs
Plans Rapidly Ramped Up Efforts to Meet Enrollees’ Needs
All the plans responding to the survey said that they conducted enrollee outreach to identify unmet needs related to COVID-19. Some plans prioritized outreach to their high-risk enrollees, with one plan describing how it developed predictive models to identify enrollees at high risk for current or near-future unmet social needs. Other plans said that they stepped up the frequency of scheduled (now virtual) contacts with enrollees. Plans also identified social needs through enrollee interactions with care management staff (85% of plans), outreach to the plan from enrollees (77% of plans), referrals from community-based organizations (CBOs) and social service agencies (31% of plans), and provider referrals (15% of plans). One plan reported creating specialized roles for health outreach workers to assess enrollee needs.
Access to food was the most commonly reported need, and many plans described their efforts to address this problem, which included:
- Development or expansion of emergency meal programs;
- Coordination and delivery of food/personal supplies from local food banks;
- Expansion of a Fresh Food Farmacy program;
- Creation of food pickup events; and
- Identification of community resources for food assistance.
Plans also reported delivering PPE to enrollees’ homes, as well as providing diapers, formula, and other essential supplies. Identifying community resources to help enrollees with housing and financial needs was also a plan priority. Several plans said that they increased outreach efforts to combat isolation and loneliness among enrollees and to identify other mental health needs resulting from the pandemic.
Community Partnerships Are Key in Meeting Enrollee Needs
ACAP-member plans rely on community partners to help address their enrollees’ social needs. This includes long-standing relationships with Meals on Wheels, county social service agencies, and transportation providers as well as partnerships with organizations such as Service Access and Management, Inc. and Benefits Data Trust that help to connect plan enrollees to the services they need.
Several plans reported that they partnered with CBOs through Aunt Bertha’s free online source, findhelp.org. They also have direct contracts with some types of service providers (e.g., transportation and meal providers), and support other types of providers (e.g., workforce training, housing supports organizations) through grants and charitable donations. In addition, plans have informal relationships with CBOs that provide items such as furniture, home repair, clothing, and rides. One plan created the Cultivating Health for Success program to provide members with supportive housing by partnering with its sister behavioral health organization, county department of human services, and a family medicine practice.
With the arrival of COVID-19, ACAP plans stepped up contracting efforts with CBOs to provide services to their enrollees, particularly related to providing food and addressing social isolation. One plan began using the Unite Us platform to create and track referrals to CBOs. Another plan expanded connections to organizations such as United Way and its 2-1-1 program to help enrollees access support for emergency basic needs. Other plans signed new contracts with providers for emergency meal service coordination and to help combat social isolation.
New Opportunities to Meet Enrollee Needs
Partnerships with CBOs are key, but given the pandemic’s effects on dually eligible individuals, health plans would benefit from additional resources to address the increasing prevalence of social needs among their enrollees. In an October 2020 report, ACAP and CHCS explored opportunities for D-SNPs to use new Medicare Advantage supplemental benefit flexibilities to help meet enrollees’ needs. Although these new flexibilities are useful to some extent, the Centers for Medicare & Medicaid Services (CMS) could consider policy options to provide D-SNPs with additional tools to address their enrollees’ social risk factors, including:
- Allowing D-SNPs to offer supplemental benefits that address social needs to a wider range of their enrollees — nearly all of whom have low incomes. Expanded access to these benefits could help address the loneliness and stress caused by COVID-19’s social distancing requirements.
- Adjusting CMS’ Star Rating quality measurement system to reflect the levels of social need among D-SNP enrollees. This could be done by redesigning Star Ratings comparison groups as recommended by MedPAC, or by allowing D-SNPs to retain a higher percentage of their rebate dollars. These adjustments could provide D-SNPs with more resources to pay for supplemental benefits such as home-delivered meals.
- Adding indicators of social need to the Medicare Advantage risk-adjustment model. Incorporating indicators of an individual’s social needs into the CMS Hierarchical Condition Category risk-adjustment model could improve the model’s accuracy and could increase payments to plans that enroll dually eligible individuals.
D-SNPs and MMPs have always served dually eligible individuals who have numerous social risk factors. During the COVID-19 pandemic, these plans have seen a significant rise in social needs among their enrollees. ACAP member plans are leveraging partnerships with CBOs and using new supplemental benefit flexibilities to address these needs. Federal-level policy changes could provide health plans with much-needed supports for vulnerable dually eligible populations.




