State Medicaid agencies are beginning to use policy levers to address well-documented, widespread disparities in health care and outcomes and address long-entrenched health inequities linked to factors such as race, ethnicity, disability status, geography, sexual orientation, and gender identity. One potentially powerful policy lever is payment reform. Combining financial incentives and alignment with strategic efforts to shift away from fee-for-service payments can help prioritize health care system investments and generate leadership buy-in to drive more equitable care delivery.
To help payers and other stakeholders make tangible progress on this front, the Health Care Payment Learning and Action Network (LAN) recently released Advancing Health Equity Through APMs: Guidance for Equity-Centered Design and Implementation. The guidance document, developed by the LAN Health Equity Advisory Team, recommends changes to alternative payment models (APM) to make care more accessible and equitable, and drive better health outcomes. It calls on public and private health care stakeholders to collaborate on implementing the approaches in an aligned manner.
To help state Medicaid agencies apply the LAN guidance and support health equity within payment reform efforts, this blog post summarizes the guidance and describes practical steps for immediate action.
Overview of Advancing Health Equity Through APMs
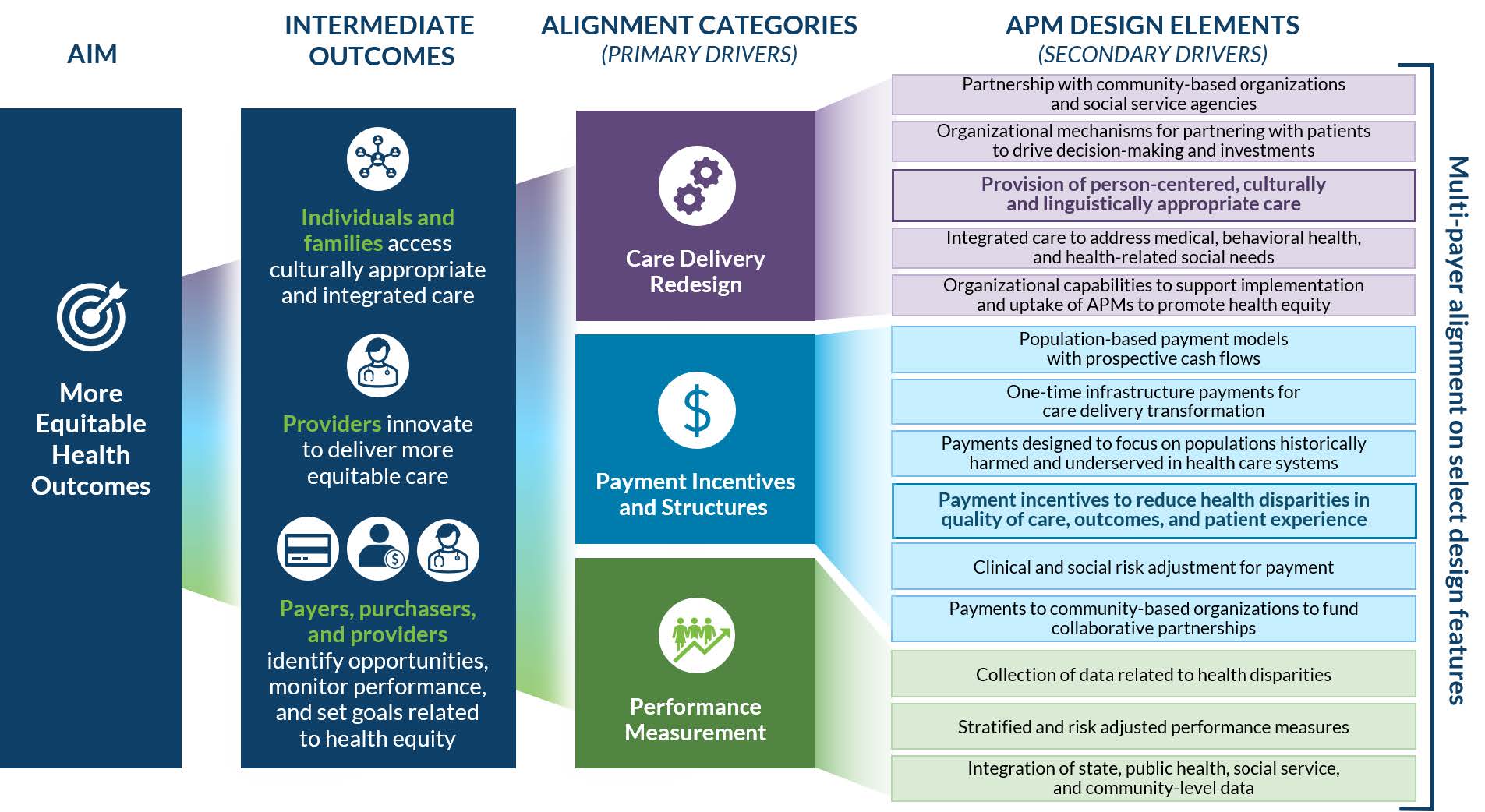
Advancing Health Equity Through APMs describes a theory of change for how APMs can advance health equity (see Figure 1) and outlines approaches for incorporating two specific design elements into APMs: (1) person-centered, culturally and linguistically appropriate care; and (2) payment incentives to reduce health disparities in quality of care, outcomes, and patient experience.
Figure 1. Theory of Change: How APMs Advance Health Equity (click to enlarge)
Source: Health Care Payment Learning & Action Network. Advancing Health Equity Through APMs: Guidance for Equity-Centered Design and Implementation. December 2021.
To promote adoption of person-centered, culturally and linguistically appropriate care models, the LAN recommends that public and private payers and purchasers modify contract terms to:
- Encourage and enable person-centered, culturally and linguistically appropriate care that integrates physical, behavioral, oral, and social health;
- Incorporate a diverse (e.g., racial diversity, diversity of lived experiences) and expanded health care workforce (e.g., doulas, community health workers) into existing care teams;
- Measure adoption of these practices using a limited set of aligned measures;
- Adjust provider payments to include both: (a) time-limited, upfront payments to support capacity building; and (b) prospective, population-based payments sufficient to support these services via an expanded workforce.
The LAN recommends that payers enhance payment incentives in the following ways:
- Create greater accountability for health equity through:
- Aligned, but limited health equity performance measures stratified by race, ethnicity, language, and other demographics based on prevalent disparities in a state or region;
- A common methodology for measuring disparities and year-over-year change;
- An adjusted scoring methodology that includes health equity as a significant percentage of a provider’s quality score; and
- Adjusted payments, upward or downward, based on improvement and/or achievement.
- Support historically under-resourced providers through:
- A separate and additional health equity bonus pool that rewards improvement;
- Time-limited upfront payment to support capacity building and practice transformation; and
- Payments that adequately cover patient care costs.
Advancing Health Equity Through APMs also includes design guidance to help stakeholders tailor these contract changes to address local context and community/provider priorities. The guidance is structured with “essential” and “enhanced” approaches for more advanced implementers, as well as examples of how Medicaid, commercial, marketplace, and Medicare payers have already adopted these recommendations. The guidance provides tips for implementation, which emphasize partnering with communities throughout the process of incorporating these elements into APMs and developing a plan for measuring unintended consequences of APM adoption.
Practical Steps for Medicaid Agencies
State Medicaid programs typically use one of two approaches to promote managed care organization (MCO) and provider adoption of value-based payment (VBP): (1) VBP adoption requirements for contracted MCOs; or (2) state-designed models that providers participate in either directly with the state or through managed care. States using either approach can begin to incorporate health equity into their APM approaches by taking the following actions in partnership with community members, providers, and MCOs:
- Establish a shared definition of health equity;
- Define health equity goals and a limited set of aligned measures used to track progress and incentivize improvement;
- Define what person-centered, culturally and linguistically appropriate care looks like, including the relevant workforce; and
- Agree on approaches to bolster the capacity of under-resourced providers that work with historically marginalized populations.
Building on these actions, states can take the following steps, based on their VBP strategy:
- States with MCO contract requirements for VBP can incorporate LAN health equity design elements into Medicaid MCO contract requirements related to VBP. Using LAN health equity guidance, states can modify their MCO VBP requirements to:
- Require all new and renewed VBP contracts to incorporate either essential or enhanced design elements and set a timeline for incorporating these elements into existing VBP contracts;
- Require MCOs to partner with patients and communities to ensure that their input is sought and incorporated into the design of care delivery and payment models;
- Adjust MCO withholds/bonus arrangements to reward MCOs that incorporate LAN health equity design elements into VBP arrangements and reduce health disparities in an aligned set of measures;
- Require MCOs to assess unintended consequences that perpetuate or increase health disparities and make modifications as needed; and
- Modify MCO VBP reporting requirements and templates to collect information about how MCOs have adjusted their VBP models to address health equity and analyses of unintended consequences.
- States with state-developed VBP models can incorporate LAN Health Equity Design Elements into VBP models. State-developed models can be modified to incorporate LAN health equity guidance, including primary care/population health prospective payments, accountable care organization (ACO) shared savings/risk, episodes of care/bundled payments, and pay for performance models. Models can be modified to:
- Incorporate LAN recommendations into APM payment methodologies, including adjusting upfront payments to support capacity building and incorporating a pay-for-reporting component in the baseline year;
- Incorporate LAN care delivery recommendations into APM contract expectations;
- Modify provider data analytics to report on stratified measurement sets and make resulting data transparent to communities;
- Collaborate with providers and community organizations to assess and improve demographic data quality, prioritizing self-reported demographic data and mechanisms for obtaining that data; and
- Monitor and address unintended consequences that perpetuate or increase health disparities.
Existing State Efforts to Address Health Equity
Medicaid agencies are already deploying approaches to advance health equity through APMs that align with LAN recommendations. For example:
To promote person-centered, culturally and linguistically appropriate care models:
- Kentucky sets contractual expectations for MCOs to recognize enrollees’ beliefs, competently address cultural differences; and foster attitudes and communications among staff and providers that respect enrollee’s cultural background.
- Oregon incentivizes access to interpreter services through a new “meaningful language access to culturally responsive health care services” incentive metric.
- Florida, Minnesota, New Jersey, New York, and Oregon cover doula services and California, Indiana, Maryland, Rhode Island, Virginia, Washington State, and Washington D.C. are moving toward coverage.
- 15 states cover community health worker services and California is pursuing a SPA to add coverage.
To reduce health disparities in quality of care, outcomes, and patient experience:
- Rhode Island incentivizes its Accountable Entities to improve collection of patient race, ethnicity, and language data.
- North Carolina provided an enhanced payment to primary care practices serving areas of the state with high poverty rates, as part of its Health Equity Payment Initiative.
- Massachusetts has proposed health equity incentives for ACOs, ACO-participating hospitals, and non-state-owned public hospitals as part of its 1115 proposal.
- California will establish a Health Equity Sub-pool in its Global Payment Program to incentivize eligible public hospitals to invest in services that reduce health inequities.
Looking Ahead
As noted by the LAN, the country is at a critical time for taking action and making tangible progress to reduce health disparities and transform health care into a more equitable system. Payment reform creates a practical opportunity for state Medicaid leaders to foster greater accountability for and make measurable improvements in health care quality for populations that experience the worst health outcomes. Advancing Health Equity Through APMs provides concrete guidance to help states and other purchasers design and implement payment approaches that can move the needle. While the process of aligning stakeholders around health equity definitions, metrics, and equitable care models is not a simple endeavor, state leaders can tap into a shared commitment to health equity to accelerate this important work.