Program At-A-Glance
Organization: Center for Youth Wellness
Description: Innovative children’s health organization within a pediatric clinic serving children and families in District 10 of San Francisco, California.
Goal: To systematically prevent and address toxic stress among children and families exposed to adverse childhood experiences.
Key Program Features: Developing and testing a new ACEs screening tool; developing initiatives to prevent secondary trauma in clinical staff; and creating a welcoming space for children and families.
Nadine Burke Harris, MD, FAAP, MPH first realized the need for trauma-informed care shortly after beginning work at California Pacific Medical Center (CPMC). Together, CPMC and Burke Harris had just opened a clinic in Bayview-Hunters Point, one of the most economically disadvantaged and geographically isolated neighborhoods in San Francisco. Despite the city’s reputation for wealth, the median household income in Bayview-Hunters Point is $30,000 per year, with 39 percent of the population living below 200 percent of the federal poverty level. Within the city, the area has disproportionately high hospitalization rates for conditions including congestive heart failure, diabetes, chronic obstructive pulmonary disorder, and asthma.
“We educate parents about the impacts of adverse childhood experiences and toxic stress the same way you would for covering electrical outlets or lead poisoning.”
Burke Harris immediately noticed that an unusually high percentage of kids were being referred to her for attention deficit hyperactivity disorder (ADHD). However, upon assessing most children for ADHD, she found that she could not make the diagnosis. Traumatic experiences seemed to be the underlying cause of many of the children’s behavioral issues. Burke Harris became interested in how trauma could be more effectively diagnosed and treated, beyond simply medicating its symptoms. As a result, the Center for Youth Wellness (CYW) was formed in 2012.
CYW has since become a national pioneer in the field of trauma-informed pediatrics through its innovative work addressing the impact of toxic stress in children. CYW’s multidisciplinary approach focuses on preventing and undoing the chemical, physiological, and neurodevelopmental results of adverse childhood experiences (ACEs). Its model integrates primary health care with family-focused behavioral health services to meet children and families where they are to support them in leading healthier lives.
Ingredients of Trauma-Informed Care
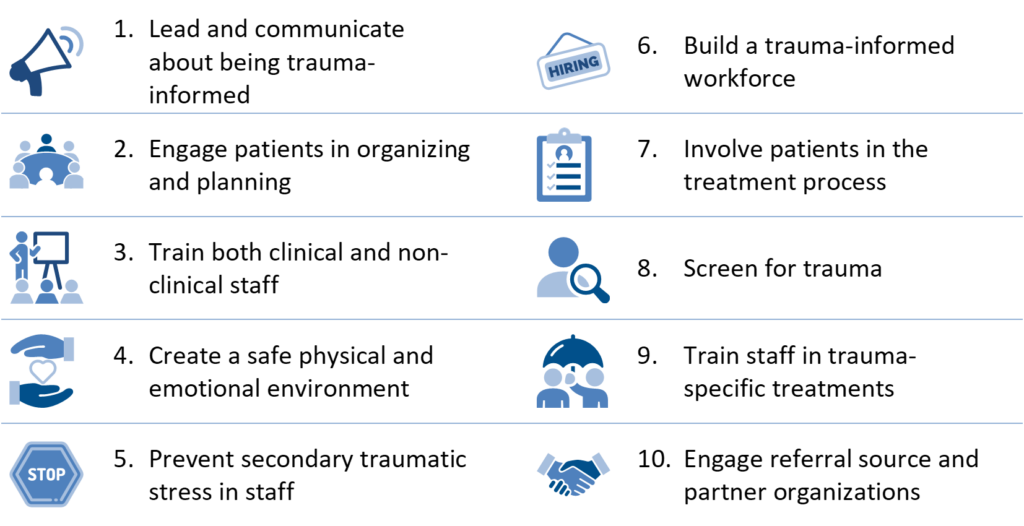
Based on expert insights, the Center for Health Care Strategies (CHCS) compiled these core organizational and clinical elements to guide practitioners in pursuing trauma-informed care. Many of these ingredients are incorporated into CYW’s approach, with select features described below.
SOURCE: C. Menschner and A. Maul. Key Ingredients for Successful Trauma-Informed Care Implementation. Center for Health Care Strategies, April 2016.
Select Features of CYW’s Trauma-Informed Approach
Based on ingredients of trauma-informed care outlined above, following are select aspects of CYW’s approach to addressing trauma.
 Leading and Communicating about the Transformation Process
Leading and Communicating about the Transformation Process
CYW’s leadership are active in building the trauma-informed care movement within their organization and beyond their walls. Burke Harris’ TED Talk, “How Childhood Trauma Affects Health Across a Lifetime,” has been viewed more than three million times, and her work has been profiled in The New Yorker, in Paul Tough’s “How Children Succeed: Grit, Curiosity, and the Hidden Power of Character,” and in Jamie Redford’s film, “Resilience.” Burke Harris also recently released a book on toxic stress and health, “The Deepest Well: Healing the Long-Term Effects of Childhood Adversity.”
In spring 2017, CYW launched the National Pediatric Practice Community on Adverse Childhood Experiences (NPPC), an initiative that aims to enhance the quality of pediatric care and improve health outcomes by integrating a toxic stress framework and ACEs screening and intervention into pediatric medicine. Over three years, the NPPC is seeking to support 1,000 pediatric medical providers across the country in making ACEs screening and intervention part of their routine clinical practice.
 Creating a Safe Physical and Emotional Environment
Creating a Safe Physical and Emotional Environment
With its bright colors and kid-sized furniture, CYW looks like most other pediatricians’ offices — cheerful. However, its light-hearted surface belies the hard work that went into the building’s development. The CYW’s partner clinics, the Bayview Child Health Center (BCHC), Safe and Sound (previously the San Francisco Child Abuse Prevention Center), and Child Advocacy Center (CAC), are all located within the same building as CYW, keeping families from having to travel back and forth to several different agencies. Additionally, several alternate entrances and exits were designed to allow for greater anonymity and discretion. In this way, CYW staff can ensure that children and families coming in for wellness services or to see a physician do not cross paths with child welfare workers or police officers participating in CAC investigations, a potentially intimidating experience.

Training Clinical and Non-Clinical Staff
CYW ensures that patient encounters with staff are as positive and reassuring as possible. Clinical and non-clinical staff (such as front desk workers, members of the development and finance teams, etc.) have participated in “cultural humility” trainings. These trainings address how culture affects the ways in which individuals perceive trauma, safety, and privacy. CYW has since included cultural humility as a core organizational value, and is committed to cultivating a welcoming place for patients and families from all racial, socioeconomic, and cultural backgrounds.
 Preventing Secondary Traumatic Stress in Staff
Preventing Secondary Traumatic Stress in Staff
CYW recognizes that caring for children who have been exposed to abuse, neglect, and other traumatic experiences can take a heavy emotional toll on staff. As such, CYW is committed to preventing secondary traumatic stress for all of its staff. They have been trained in transcendental meditation and can participate in daily “wellness breaks” and weekly wellness services such as on-site yoga. Direct care staff have also participated in Cultivating Emotional Balance, an evidenced-based meditation and emotional awareness training aimed at supporting the practice of empathic, compassionate medicine and preventing burnout. In this way, CYW attempts to address trauma on a systemic level in order to develop an overarching culture of health within the organization.
 Using Trauma-Informed Screening and Treatments
Using Trauma-Informed Screening and Treatments
A sign in BCHC’s patient waiting room makes it clear — “We Ask Everyone.” Each caregiver, child, and teen seen by the doctor receives an ACEs screening assessment from a trained medical assistant. Normalizing the asking helps to eliminate the shame that people may feel about exposure to adverse experiences. CYW developed its own screening tool, the ACE-Q, which screens for factors in the original ACE questionnaire, as well as community violence, time in foster care, and mistreatment due to racism/discrimination. The scores are reviewed with the patient and his or her caregiver. BCHC’s pediatric primary care providers (PCPs) use these scores to assess risk of toxic stress physiology: “I know that if my patient has an ACE score of 4, she’s two and a half times as likely to develop hepatitis or COPD; four and half times as likely to become depressed; and 12 times as likely to attempt to take her own life as a patient with zero ACEs. I know that when she’s in my exam room,” says Burke Harris.
The screening process provides a valuable opportunity to discuss the effects of ACEs and toxic stress with parents, regardless of their child’s score. If a patient receives a score of 4 or higher (or 1-3 with symptoms), the PCP will recommend an integrated care plan that includes referrals to a team of psychotherapists, psychiatrists, care coordinators, and other trained experts. These providers will discuss how to avoid exposure, manage stress, and build supportive relationships.
Next Steps for Trauma-Informed Care at CYW
While CYW is at the national forefront in the field of pediatric trauma-informed care, it also continues to refine practices for the children and families it serves. For example, CYW is in the process of updating its electronic health record to more easily facilitate the development of integrated patient treatment plans and effectively track patient progress.
More broadly, CYW is identifying ways to advance the field nationally by supporting ACEs research and physician training through the NPPC network. Additionally, CYW recently launched Stress Health, a national campaign aimed at building awareness among parents and caregivers of the impact of toxic stress and encouraging early intervention. Through these efforts, CYW is making a difference not only in the lives of local children and families, but bringing attention to the issue of toxic stress nationwide. As Burke Harris notes: “We are trying to make sure that no one has to wonder what might have happened if they screened for trauma earlier.”
Trauma-Informed Care in Action Profile Series
This profile series features participants in Advancing Trauma-Informed Care, a national demonstration project designed to better understand how trauma-informed approaches can be practically implemented within the health care sector. LEARN MORE »