Program Snapshot
Name: ThedaCare
Goal: Improve high-risk patients’ health care outcomes by delivering services to their homes.
Featured Services: Deploy community paramedics to the homes of medically and socially complex patients to review medications, address social needs, and support patient self-management.
Target Population: Participants must have: (1) three or more emergency department visits in the past six months (or six in 12 months); and/or (2) recent inpatient hospital admissions; and/or (3) home safety and/or medication concerns, or other issues as identified by a primary care physician. Those ineligible include patients already receiving medical care through home health visits.
Brian Randall is a paramedic in northeastern Wisconsin, but when he goes out on a call he does not careen down the street in an ambulance, sirens blaring and lights flashing. Instead, Randall, who meets with people with complex medical and social needs in their homes, drives a Suburban and is more likely to be carrying a weighted lap blanket or blood pressure cuff than a stretcher. He is one of two community paramedics from Gold Cross Ambulance Service who work in partnership with ThedaCare, a large nonprofit health care system in Wisconsin, to bridge existing gaps in chronic disease management for patients struggling to manage their health.
ThedaCare serves 235,000 residents in the Fox Cities region of Wisconsin. In 2016, ThedaCare was one of six organizations selected to participate in the Transforming Complex Care (TCC) initiative, made possible through support from the Robert Wood Johnson Foundation and led by the Center for Health Care Strategies (CHCS). Under the TCC initiative, ThedaCare sought to extend the reach of its clinics to serve the most medically and socially complex patients through a community paramedicine pilot program. The community paramedics work in partnership with ThedaCare’s Ambulatory Care Management team and departments within the hospitals to identify patients who would most benefit from the program.
COMPLEX CARE INNOVATION IN ACTION
This profile is part of an ongoing series from CHCS exploring strategies for enhancing care for individuals with complex health and social needs within a diverse range of delivery system, payment, and geographic environments. LEARN MORE »
Building a Business Case for Community Paramedicine
The goal of ThedaCare’s program is to reduce over-utilization of emergency department (ED) and hospital services, and the associated high costs. ThedaCare began piloting its team-based care model for Medicare patients in 2014. At the time, ThedaCare, as part of the Centers for Medicare & Medicaid Services’ Pioneer Accountable Care Organization Model, was evaluated on its ability to deliver on the Institute for Healthcare Improvement’s Triple Aim: better care for individuals, better health for populations, and lower growth in expenditures. After patients with the highest utilization of costly emergency and hospital services were identified, they were connected to a care team. The team, including a registered nurse care coordinator, a pharmacist, and a social worker, worked closely with primary care physicians to provide intensive case management, and referrals to social services. The team also offered home visits for patients who had medication issues or faced other impediments to managing their health.

But, says Sandi Groenewold, MD, ThedaCare’s Expanded Care Team Physician Lead, the program found that “Not many patients were interested in having a doctor or nurse come to their homes. They preferred to meet their clinicians in the clinic, if at all.” Groenewold, who now manages ThedaCare’s community paramedicine program, had heard about other groups across the country using community paramedics for home visits with complex care patients, and became intrigued with the concept. She and other members of the care team met with Gold Cross, an ambulance service operating over 2,100 square miles in northeastern Wisconsin that was also exploring the how to better serve medically and socially complex patients. “Adding a community paramedic has allowed us to reach patients who we were not reaching before,” says Groenewold. “Community paramedics are used to going into people’s homes in difficult situations and they are very relaxed and calm during home visits.” This finding is not unique to ThedaCare’s program; community paramedics have been well received in rural areas and in other home visiting contexts, and evidence is building that patients have a comfort level with them that they may not have with other care team members.
“There are times when we hear from the primary care setting that they have an intuitive feeling that something is off, something is wrong, and they ask us, ‘Can someone go in and see what’s going on with this patient?’”
ThedaCare’s community paramedics complete a certified community paramedic program, including two semesters of coursework in primary care, preventive health, wellness, and management of chronic diseases such as diabetes and high blood pressure, and 196 hours of clinical training. They help close gaps in care for some of the highest-risk complex care patients: those who, due to significant social and emotional issues, are not only experiencing serious challenges managing their health, but are also difficult to reach.
Establishing ThedaCare’s Community Paramedicine Program
A key initial step in building the community paramedicine program was conducting a gap analysis to make sure the program was able to reach people with the greatest care needs that were not being met by other programs. “We did not want to compete with home health, other care management services within the ThedaCare organization, or other community services” says Groenewold. “We really wanted to focus on those whose needs we just weren’t meeting.”
The criteria for who is served through ThedaCare’s community paramedicine program evolved over the course of the pilot. Initially, patients had to have made three or more visits to the ED in six months, or six or more over the course of a year to participate. Eventually, primary care physicians also began referring patients about whom they had serious concerns, i.e., a patient who was not taking her prescribed medications correctly; a patient who had multiple clinic and specialist visits, yet still seemed confused about managing her health; or a patient whose adult children called multiple times with concerns about their parent. “There are times when we hear from the primary care setting that they have an intuitive feeling that something is off, something is wrong, and they ask us, ‘Can someone go in and see what’s going on with this patient?’” says Groenewold. The program partners with inpatient care units in two regional hospitals in the Fox Valley area, so nurses are able to connect patients with care teams and make referrals for community paramedic home visits if there are concerns about medications or readmissions, or just a “gut feeling” that something does not fit the clinical picture.

Since launching in 2017, ThedaCare’s community paramedicine program has expanded from one part-time community paramedic to one full- and one part-time paramedic based on the program’s success. As of March 2018, nearly 150 patients have been served by the community paramedics, with 30-40 served at any given time. Roughly 85 percent of patients referred to the community paramedicine program are covered by Medicare, Medicaid, or are dually eligible for both programs, though a few are privately insured. Most of the patients have multiple chronic conditions such as diabetes, heart failure, or chronic obstructive pulmonary disease. Plus, many have some type of behavioral health condition that has not always been diagnosed. “Social determinants of health (SDOH) play a significant role with this population,” says Groenewold, who adds that the TCC pilot helped to create relationships with a range of community partners involved in housing, food security, and mental health services.
Connecting the Home to the Clinic
Community paramedics are fully integrated into ThedaCare’s Ambulatory Care Management team, working with nurses, the primary care physician, the clinical pharmacist, and any external services like physical therapy or occupational therapy. Randall has access to all patients’ information through an electronic health record (EHR) that includes an SDOH assessment tool. “We see people in their home setting where we can really get a full view of their life,” says Randall. The electronic assessment tool, which was developed by ThedaCare under TCC, helps the care team identify a range of factors that may be impacting a patient’s health and wellbeing, such as medication concerns, safety issues in the home, and food security. “I ask every single one of my patients, ‘Do you have problems getting food in your home?’” says Randall. “You’d be amazed at how many say yes and just don’t have the resources to get that corrected.” Randall also inquires about life hazards, such as whether people wear seatbelts, work in transportation, or in a job where they are exposed to lots of chemicals; do they live in an unsafe community or area with a high crime rate; or do they have concerns about their personal safety?
“I ask every single one of my patients, ‘Do you have problems getting food in your home?’ You’d be amazed at how many say yes and just don’t have the resources to get that corrected.”
The Community Paramedic Program operates from 6:45 am to 8 pm, Monday through Friday, to accommodate the schedules of most patients. Depending on the reason for the referral, patients may be seen once or several times, with the goal of gradually moving them toward independently managing their health. Paramedics record what resources they linked a patient to and which interventions they provided — such as education around diet, diabetes, or preventing infections — directly in the EHR in real-time during home visits. This record gives the members of the overall care team a clearer picture of their patients’ health and informs the care they provide. It also provides patients with a cohesive set of instructions and a better coordinated care plan.
In many ways, community paramedics are problem solvers — a skill that carries over from emergency medical training. “We’ve seen people who stop taking all their medications because they lost their insurance and they didn’t tell anybody because they were either embarrassed or didn’t know what to do,” says Randall. Community paramedics can help patients apply for Medicaid or state aid, and if they do not qualify and there are no other options, Randall, works to identify alternatives. “I’ll go through their medication list and say, ‘These are on the four dollar list at Walmart, and these three, we’re going to get through mail order because they’re pennies on the dollar.’”
Using a motivational interviewing approach is an important part of the job, says Groenewold, who adds that some of the patients who receive home visits are resistant to change. After training in motivational interviewing, ThedaCare’s community paramedics are able to have non-confrontational conversations with patients that help them identify what is important to patients as well as their ability and readiness to do something about it.
That was the case with one 65-year-old man with Type 2 diabetes who was referred to the program after testing revealed a hemoglobin A1C (HbA1C) level above 9.0, putting him at increased risk of heart failure, nerve damage, and other diabetes-associated complications. The patient had recently been denied hip replacement surgery due to the risks associated with uncontrolled diabetes. He was in great pain, severely overweight, and struggled to exercise or even sit for extended periods of time. Despite having met with a diabetes educator in the past, he had problems adhering to a weight loss plan and to his complicated medication regimen.
Upon meeting with the man, Randall keyed in on the surgery as a goal for his patient to work toward. Sitting down with both him and his wife (who cooked all of their meals), Randall discussed diet modifications to help them enjoy meals while avoiding excess carbohydrates and sweets. He also reviewed exercise options that would not aggravate the man’s hip injury, such as water aerobics. Lastly, as the patient lost weight, Randall helped reduce his number of diabetic medications from four (including two injectables) to one daily pill.
After losing over 40 pounds and achieving his HbA1C goal of <7.5, the patient was approved for surgery and has consistently attended all follow-up and physiotherapy appointments. Citing the extra one-on-one time he spends with each patient, Randall says: “We reinforce the education given in the clinic or the health system. The support and time we spend in the home allows us to be more successful.”
Taking a Trauma-Informed Approach to Care
In 2014, when ThedaCare first began using a team-based model for complex care patients, “we discovered that many of the patients who really struggled with managing their health had experienced some type of trauma in their past, whether that was physical, emotional, or sexual abuse as a child, or had a really unstable family situation growing up,” says Groenewold. There is growing acknowledgement that these adverse childhood experiences can impact an individual’s ability to take control of their health and interact with the medical community.
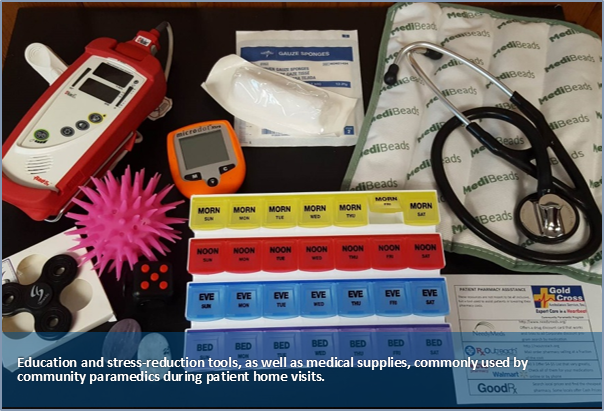
In response, the community paramedicine program takes a trauma-informed approach to care, using motivational interviewing to learn what is important to patients and identify their health care and personal life goals. Paramedics bring sensory aides such as weighted blankets, worry stones, and fidget tools to home visits to help calm patients experiencing anxiety. “We call our approach ‘kindness with boundaries,’” says Groenewold. “We hold patients accountable, but involve them in creating realistic expectations.” The paramedics also hold off on judging patients when they miss appointments or act out, instead they try to figure out what triggered the outburst. Approaching people in this way helps the team build strong, trusting relationships that ultimately help them be more successful in their health and improves communication with clinicians.
Sustaining the Model
At present, community paramedic services are not reimbursed by Medicare, Medicaid, or private insurance. However, as evidence grows that community paramedics can help improve outcomes and reduce utilization of costly services by bridging gaps in care, there is growing interest in expanding this service across other ThedaCare programs.
“The community paramedicine program has provided a breakthrough in terms of delivering resources to patients where the majority of their care is provided — in their homes.”
Data from the pilot’s first year indicate that adding paramedics to the care team has had a positive impact on costs and outcomes. ThedaCare is beginning to examine how its community paramedicine program might align its measures and outcomes with its accountable care organization, making it a treatment strategy for patients with complex needs. The TCC pilot is collecting data on outcomes for patients enrolled in the community paramedicine program, such as 30-day readmissions rates, ED visits, and the number of missed appointments, as well as HbA1C measures. A formal evaluation of both quantitative and qualitative data will be conducted at the project’s conclusion. Notably, legislation recently signed by Wisconsin’s governor will eventually allow licensed community paramedics to be recognized as distinct health care practitioners.
Groenewold and Randall are passionate about keeping community paramedics as integral parts of ThedaCare’s care management program. They know community paramedicine has been critical to identifying the true, underlying causes of illness for patients whom, until now, they have been unable to reach. Says Randall, “the community paramedicine program has provided a breakthrough in terms of delivering resources to patients where the majority of their care is provided — in their homes.”
Author Naomi Freundlich is a journalist with more than 25 years of experience writing about health care.
About the Center for Health Care Strategies
The Center for Health Care Strategies (CHCS) is a nonprofit policy center dedicated to improving the health of low-income Americans. It works with state and federal agencies, health plans, providers, and community-based organizations to develop innovative programs that better serve people with complex and high-cost health care needs. To learn more, visit www.chcs.org.
About Transforming Complex Care
AccessHealth Spartanburg is part of Transforming Complex Care, a multi-site demonstration aimed at refining and spreading effective care models that address the complex medical and social needs of high-need, high-cost patients. This national initiative, made possible with support from the Robert Wood Johnson Foundation and led by CHCS, is working with six organizations to enhance existing complex care programs within a diverse range of delivery system, payment, and geographic environments. For more information, visit www.chcs.org/transforming-complex-care.




