Health care professionals across the country increasingly realize the value of acknowledging trauma to improve care for patients in need. Drs. Briggs and Machtinger are participants in Advancing Trauma-Informed Care, a national initiative led by the Center for Health Care Strategies (CHCS) and made possible through support from the Robert Wood Johnson Foundation. Through the collaborative, leading national champions of trauma-informed care are exploring how trauma-informed approaches can be practically implemented across the health care sector.
Exposure to trauma, including physical, emotional, or sexual abuse; neglect; discrimination; violence; and other adverse events can impair a person’s coping skills and lead them to adopt health-risk behaviors — for example, tobacco use, drug and alcohol abuse, or risky sexual behavior. Patients who have experienced trauma may find it hard to trust other people and may be uncomfortable in a clinic setting and/or resistant to following medical advice. Studies have documented a clear link between trauma and an individual’s long-term risk for health problems.
How can Providers and Health Care Delivery Systems Become Trauma-Informed?
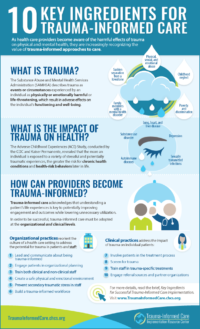
Recognizing the negative impact of trauma on health is just the first step for health care organizations in better addressing the care needs of patients who have experienced trauma. Adopting trauma-informed approaches to care can equip health care organization with tools to more effectively address the needs of these patients. To be fully effective, trauma-informed care must involve both organizational practices and clinical practices. Organizational practices reorient the culture of a health care setting to address the potential for causing trauma in patients and staff, while trauma-informed clinical practices address the impact of trauma on individual patients.
Drawing from the insights of experts across the country, CHCS developed a set of key ingredients to guide health care organizations in adopting best clinical and organizational practices for addressing trauma-informed care. Following are the key ingredients and examples for each:
Organizational Ingredients for Trauma-Informed Care
- Engage patients in organizational planning. Invite patients with lived experience of trauma to join a stakeholder committee and help guide effective implementation of trauma-informed care.
- Train clinical as well as non-clinical staff members. Assist clinical as well as non-clinical staff, such as security guards and front-desk workers, in fostering a welcoming, trusting, and non-judgmental environment, including training on how to de-escalate tense situations.
- Create a safe physical and emotional environment. Provide a calm, quiet waiting room and exam space, and ensure that patients feel respected.
- Prevent secondary traumatic stress in staff. Invest in staff wellness through trainings, mental health days, a focus on self-care, etc., to reduce the potential for staff burnout.
- Hire a trauma-informed workforce. Use behavioral interviewing techniques to look for key qualities in job candidates, such as empathy, non-judgment, and collaboration.
Clinical Ingredients for Trauma-Informed Care
- Engage patients in the treatment process. Involve patients in decision-making and the development of their care plan, rather than dictating the course of action.
- Screen for trauma. Determine the best screening tools and methods to use based on the health care setting and patient population.
- Train staff in trauma-specific treatment approaches. Identify and train staff using an evidence-based model that best meets the needs of your organization’s care model and population served.
- Engage referral sources and partner organizations. Work with community partners and within a system of care to develop a robust trauma-informed referral network.
Promoting Trauma-Informed Approaches to Care
Leading health care professionals across the nation are recognizing the value of a trauma-informed approach to care. Understanding and adopting a trauma-informed approach to care — at both the clinical and organization level — is a key step for acknowledging the “elephant in the exam room” and more effectively addressing the needs of both patients and staff.
 ADDITIONAL RESOURCES
ADDITIONAL RESOURCES
- Trauma-Informed Care in ACTION – Brief profiles and champion perspectives from Advancing Trauma-Informed Care pilot sites that are testing innovative strategies to improve care for individuals with a history of trauma.
- Key Ingredients for Trauma Informed Care – A fact sheet, infographic, and slide presentation outlining practical steps for implementing trauma-informed approaches in a health care setting.
- Understanding the Effects of Trauma on Health – A fact sheet and slide presentation exploring the causes of trauma and how it can impact an individual’s health.
These resources are a product of Advancing Trauma-Informed Care, a national initiative aimed at understanding how trauma-informed approaches can be practically implemented across the health care sector, made possible through support from the Robert Wood Johnson Foundation.
For additional resources, see also:
- ACESTooHigh – This news site reports on adverse childhood experiences research and how stakeholders across the country are implementing evidence-based, trauma-informed practices.
- Mobilizing Action for Resilient Communities – This collaborative of 14 communities across the country is working to build a culture of health by translating the science of adverse childhood experiences into practices and policies that foster resilience.




