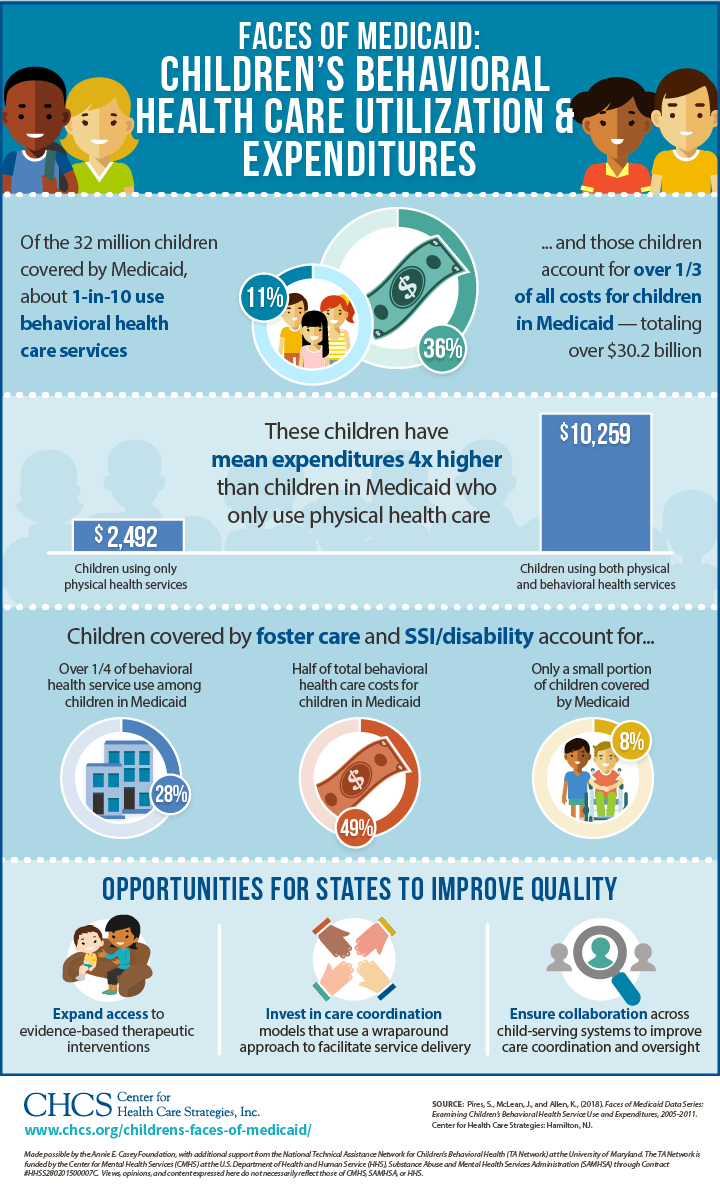
Children in Medicaid with behavioral health needs are one of the program’s most vulnerable populations — representing a small portion of the Medicaid child population, but accounting for disproportionate costs. These children are often served by multiple public programs, putting them at risk for fragmented or uncoordinated care, and they often experience poor health outcomes at high costs. This infographic is a companion to the Center for Health Care Strategies’ (CHCS) national analysis of 2011 Medicaid claims data, available as part of CHCS’ ongoing Children’s Faces of Medicaid data analysis series.
*The National Technical Assistance Network for Children’s Behavioral Health at the University of Maryland is funded by the Center for Mental Health Services (CMHS) at the U.S. Department of Health and Human Services (HHS), Substance Abuse and Mental Health Services Administration (SAMHSA) through Contract #HHSS280201500007C. The views, opinions, and content expressed here do not necessarily reflect the views, opinions, or policies of CMHS, SAMHSA, or HHS.




