Program At-A-Glance
Organization: Women’s HIV Program at the University of California, San Francisco
Description: Integrated primary medical care, social work, and mental health services in a Ryan White primary care clinic serving women and girls living with HIV.
Goal: To study the impact of a holistic model of trauma-informed primary care on the physical and behavioral health outcomes of patients and the experience of providers.
Key Program Features: Incorporating “patient voice” into all aspects of organizational and treatment processes; forming an advisory board of patients and staff; trainings with regular follow-up to create a trauma-informed culture; regular interdisciplinary team meetings; and individual/group treatments for past trauma, post-traumatic stress disorder, and substance use, available onsite and via referrals to trusted partners.
When the Women’s HIV Program at the University of California, San Francisco (WHP) opened in 1993, medical science had little to offer in the fight against AIDS. The clinic’s patients — low-income women, almost all with a history of poverty, violence, and/or substance use — would likely die from the disease. As a federally funded Ryan White HIV/AIDS Program, the clinic did what it could with an ahead-of-its-time model of coordinated care that leveraged medical care and essential social services to help patients be healthy and well. But patients’ outcomes remained grim.
Fortunately, by the time Edward Machtinger, MD (Dr. Eddy to patients) arrived at the clinic in 2000, becoming director shortly thereafter in 2004, things began to change. Medical science scored some important victories against HIV/AIDS and the introduction of antiretroviral drugs promised to drastically reduce mortality linked to the virus.
“It’s hard to overstate the impact of having services to address what I feel is the primary underlying issue faced by most of the women in clinic, which is trauma.”
When Machtinger began treating women at the WHP clinic, however, he noticed an alarming trend — although markers of patients’ HIV/AIDS were being kept in check, their overall health was deteriorating. Then, the murder of a beloved patient shocked the clinic into reexamining how it addressed the health impacts of issues such as intimate partner violence (IPV) and addiction. Machtinger and his colleagues began analyzing program data from the past 10 years, uncovering surprising findings: only 16 percent of WHP patients who had died had succumbed to complications related to HIV/AIDS. The remaining deaths were a result of trauma and its sequelae, such as physical abuse, substance use, or suicide. HIV/AIDS was no longer the primary problem facing WHP’s patients; it was the trauma in their lives. This “aha” moment led WHP to search for new ways to confront the trauma underpinning so many of their patients’ problems.
Today, patients have a voice in almost every aspect of WHP’s operations, from how trauma screenings are performed, to the atmosphere of the clinic waiting room. To further refine its model of trauma-informed primary care, WHP is conducting an ongoing, comprehensive implementation study to identify which trauma-informed practices have the greatest positive impact on patient and provider satisfaction and to identify gaps. Recently, for example, to supplement mental health services, a clinician from the Trauma Recovery Center at San Francisco General Hospital, a world-renowned program for victims of trauma, began seeing WHP patients to provide access to trauma-specific behavioral health treatments.
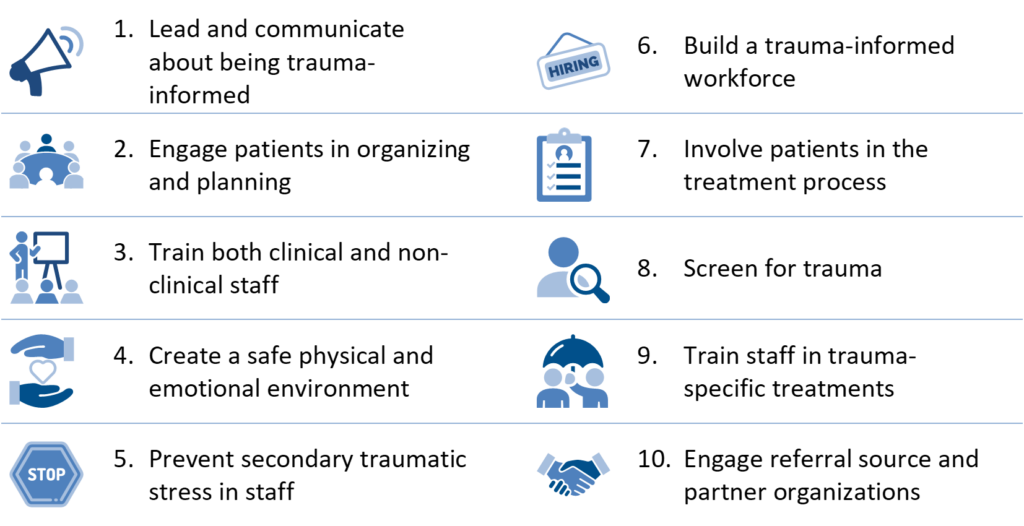
Ingredients of Trauma-Informed Care
Based on expert insights, the Center for Health Care Strategies (CHCS) compiled these core organizational and clinical elements to guide practitioners in pursuing trauma-informed care. Many of these ingredients are incorporated into WHP’s approach, with select features described below.
SOURCE: C. Menschner and A. Maul. Key Ingredients for Successful Trauma-Informed Care Implementation. Center for Health Care Strategies, April 2016.
Select Features of WHP’s Trauma-Informed Approach
Based on ingredients of trauma-informed care outlined above, following are select aspects of WHP’s approach to addressing trauma.
 Developing a Model of Trauma-Informed Primary Care
Developing a Model of Trauma-Informed Primary Care
In 2013, WHP, in partnership with Positive Women’s Network-USA, a leading advocacy organization for women living with HIV, co-convened a national working group to develop an evidence-informed model of trauma-informed primary care. The group, which included representatives from the government, military, federal agencies, academia, community organizations, and people with lived experiences of trauma, developed a model that is serving as the basis for WHP’s ongoing trauma-informed care implementation study. Through this work, Machtinger and other members of the WHP team are now outspoken advocates of trauma-informed primary care, partnering with federal agencies and speaking at conferences across the country about the promise it holds for improving care for many different populations of patients who have experienced trauma.
 Engaging Patients in Organizational Planning
Engaging Patients in Organizational Planning
When WHP’s team first began planning how to make their practice trauma-informed, it turned to Naina Khanna, executive director of the Positive Women’s Network — USA. WHP funded Khanna to conduct patient focus groups to identify: (1) how, when, and by whom women want to be screened for trauma; (2) the types of trauma-specific services that patients want, and how these should be implemented; (3) ways to ensure more meaningful involvement of patients in the implementation of trauma-informed primary care; and (4) other issues affecting women’s ability to heal from trauma.
Each focus group included participants with past and current substance use disorders, histories of IPV, as well as those experiencing post-traumatic stress disorder (PTSD). Recommendations stemming from the focus groups included strategies for meaningful incorporation of patient feedback into the clinic’s trauma-informed primary care implementation process.
 Training Clinical As Well as Non-Clinical Staff Members
Training Clinical As Well as Non-Clinical Staff Members
WHP also invited Allison Briscoe-Smith, PhD, a child psychologist with extensive experience in trauma-informed care and implicit bias, to facilitate a series of trauma-focused trainings for all staff and partners from collaborating agencies. Over three half-day training sessions, Briscoe-Smith led WHP’s staff through discussions on topics such as the impact of trauma on general health and well-being, and strategies for treating patients with complex issues such as substance use and mental health disorders. One goal of these trainings was to help staff see past patients’ sometimes disruptive behavior, and to optimize communication among team members. Briscoe-Smith subsequently provided five hour-long follow-up trainings over 12 months, focusing on practical issues faced by the clinic team such as deescalating conflicts with patients. Her initial trainings were digitally recorded so new staff may watch them when joining the team.
 Creating a Safe Physical Environment
Creating a Safe Physical Environment
One specific goal of Machtinger and the WHP team was to make the clinic’s lobby and waiting room less chaotic. Behind the scenes, they adjusted the schedule and flow of patients through the clinic and empowered receptionists and medical assistants to help patients in the moment – even if they were upset – without escalating the incident to the nurse manager. The waiting room now includes massage chairs to help patients relax before their appointment, group acupuncture, and a therapy dog from the San Francisco Society for the Prevention of Cruelty to Animals. Based on feedback from patients participating in WHP’s monthly stakeholder meetings, WHP is planning additional physical changes to make the clinic’s waiting area more welcoming, including lowering the height of the front desk so patients can more comfortably and equitably interact with staff.
 Supporting a Healthy Workforce
Supporting a Healthy Workforce
The risk for vicarious traumatization and burnout among the WHP staff is high: they often witness grave illness and distress, and frequently hear stories of mistreatment and abuse from patients. In addition, from WHP’s research, it has identified that many of its staff and providers have had traumatic experiences themselves and could be more susceptible to being triggered by working with traumatized patients. For that reason, trainings involve teaching staff the importance of maintaining appropriate patient/provider boundaries, and how to mitigate the risks for vicarious trauma and burnout among health professionals. One practice that staff have adopted to counteract stress is the “mindful minute.” The team starts their morning clinical huddle by taking a minute to breathe, relax, and get ready for the day’s work ahead. The mindful minute has been so well-received by staff that some care team members have begun convening 15 minutes early to engage in a longer group meditation.
 Involving Patients in the Treatment Process
Involving Patients in the Treatment Process
WHP is continuously evolving its clinical practices to better suit patient needs. During the focus groups, patients disclosed that they did not want physicians to screen them for substance use. Patients were concerned about their privacy, being negatively judged by the staff, and possible legal repercussions. After clarifying that physicians must know a patient’s substance use history in order to protect their health, the patients and clinic staff came up with a compromise: physicians could screen for substance use, but would need to provide clear rationale for asking such a private question, should not disclose a patient’s status unless absolutely necessary, and should screen everyone equally. This small change has made many patients feel more comfortable with disclosing sensitive information to their provider.
 Using Trauma-Informed Screening and Treatment
Using Trauma-Informed Screening and Treatment
In recognition of the high rates of IPV among clinic patients, WHP provides universal education about healthy and unhealthy relationships, the ways in which IPV affects health, and resources such as a safety card created by Futures Without Violence, a local nonprofit dedicated to ending violence against women and children. This tool provides patients with useful information about how to take care of themselves even if they are not ready to disclose they are in an abusive relationship. Patients who disclose being in an abusive relationship are immediately seen by a clinic social worker who can create a safety plan and connect them to IPV resources as needed.
WHP also has an array of trauma-specific interventions to help patients heal from the various impacts of childhood and adult trauma. Referrals to these interventions are coordinated by the WHP psychosocial team so that patients are matched with the appropriate therapy for their desires, needs, social support, and readiness. For example, WHP’s social workers oversee a group intervention for PTSD called Skills Training in Affective and Interpersonal Regulation (STAIR). The WHP team feels especially optimistic about the potential of STAIR – an adult therapy program comprised of 12, two-hour sessions that focuses on developing skills to handle triggers and mitigate the symptoms of PTSD – for their patients. In one early success, Machtinger notes a young woman he has known since she was a toddler – the daughter of a patient who completed STAIR – who shared that her mother is now much better able to control her anger. The patient also expressed that she felt relieved after learning of the impact that trauma had on her feelings and relationships, and is learning skills to cope with it.
Next Steps for Trauma-Informed Care at WHP
As mentioned earlier, WHP is conducting a multi-year study of their transformation into a trauma-informed primary care clinic. The study, now in its third year, involves a comprehensive baseline assessment of both patients and providers prior to educating WHP’s staff on trauma-informed care or integrating any new screening or interventions. Through the study, WHP is seeking to identify the intervention variables with the greatest impact on patient and provider satisfaction in order to refine their program approach. Ultimately, WHP hopes to use the study results not only to improve its own model, but also to inform larger implementation studies and efforts to help other primary care clinics and systems become trauma-informed.
Trauma-Informed Care in Action Profile Series
This profile series features participants in Advancing Trauma-Informed Care, a national demonstration project designed to better understand how trauma-informed approaches can be practically implemented within the health care sector. LEARN MORE »