Program Snapshot
Name: ReSource Teams
Goal: Use technology to assist community health workers and volunteers in connecting patients in isolated rural areas to health care providers and community resources.
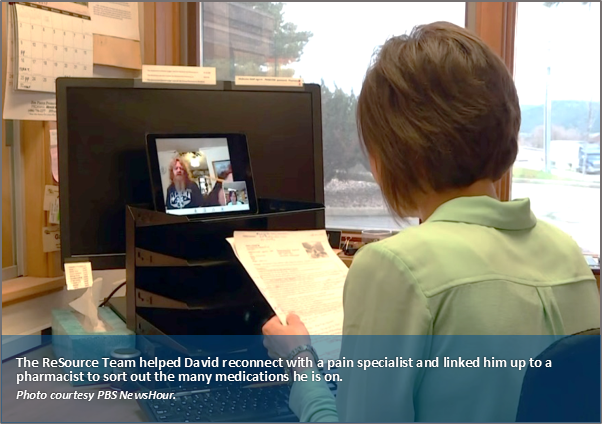
Featured Services: Piloting monthly video conferencing calls and the use of iPads during home visits to coordinate care and consult with experts.
Target Population: Participants must have: (1) two or more hospital admissions within the past six months; and/or (2) two or more emergency department visits within the same time period. Those eligible include uninsured patients, as well as those covered by Medicare, Medicaid, commercial insurance, Veteran’s Health Administration, and Indian Health services.
Montana’s Flathead Valley, a vast area in the northwestern part of the state, is the size of Connecticut, but is home to fewer than 94,000 residents. It is not unusual for people to live 30 or more miles from the closest hospital in Kalispell, the commercial center of the county. And with public transportation unavailable beyond the city limits, some of the region’s most medically complex residents have great difficulty getting to medical providers or accessing essential social services. When they do show up in the health care system, they are frequently in acute distress due to missed opportunities for ongoing preventive care. With such limited access to resources, many are simply unable to manage their complex conditions.
COMPLEX CARE INNOVATION IN ACTION
This profile is part of an ongoing series from CHCS exploring strategies for enhancing care for individuals with complex health and social needs within a diverse range of delivery system, payment, and geographic environments. LEARN MORE »
Barriers to Healthy Outcomes
Transportation is just one barrier facing Flathead Valley residents and others throughout rural Montana. Affordable housing is scarce and many high-need patients in Montana struggle with food insecurity, health literacy, and financial barriers that prevent them from getting healthy foods, medical equipment, and needed medications. The state also has long-standing shortages in its health care workforce — particularly among advanced practice nurses, primary care doctors, and behavioral health professionals — further impeding access to care.
The human and economic costs resulting from unmet social and medical needs of the state’s most vulnerable patients are stark: Mountain-Pacific Quality Health (Mountain-Pacific), a nonprofit corporation that partners with health care providers, practitioners, stakeholders, and patients on quality improvement initiatives in Montana, reports that one percent of their patients account for 22 percent of health care costs, largely attributable to multiple hospital admissions and ED visits.
For the majority of these patients, physical and social isolation directly contribute to poor health outcomes and high utilization of hospital services. “We see people who live miles away from services,” says Terry, a 69-year-old volunteer with ASSIST, a Kalispell-based organization that works with Mountain-Pacific to coordinate home visits and other services for patients dealing with complex medical and social issues. “They are struggling with unstable housing and social isolation, and are concerned about losing their ability to take care of themselves. They have no family around but have a lot of pride and don’t want to accept a handout.”
Combining High-Touch with High-Tech to Reach At-Risk Montanans
With these concerns in mind, Lara Shadwick, Mountain-Pacific’s former regional program director in Missoula, Montana, had the idea of building interdisciplinary care teams that rely on community health workers (CHW) and volunteers like Terry to visit isolated patients in their homes and help connect them to services. “Most of the models for care teams in the literature are urban-based,” says Shadwick. “We needed to find what would work with our health care workforce deficiencies and large geographic distances.” Mountain-Pacific’s “ReSource Teams” are managed by registered nurses and include CHWs and local volunteers who make home visits, as well as pharmacists and behavioral health providers who consult on medication management and behavioral health issues, respectively.
“Most of the models for care teams in the literature are urban-based. We needed to find what would work with our health care workforce deficiencies and large geographic distances.”
Two years ago, Mountain-Pacific received a $1 million innovation award from the Center for Medicare & Medicaid Innovation to use ReSource Teams to manage the care of high-need, high-cost Medicare patients in Billings, Kalispell, and Helena, Montana. Last year, additional support through the Robert Wood Johnson Foundation and the Center for Health Care Strategies’ Transforming Complex Care (TCC) initiative allowed Mountain-Pacific to expand the ReSource Team approach to Medicaid and uninsured patients, as well as those covered by commercial insurance, the Veteran’s Health Administration, and Indian Health Services. The pilot targets patients who have been admitted to the hospital two or more times within the past six months or have multiple ED visits in the same time period, as well as high-need patients referred by physicians.
To address Montana’s geographic challenges, Mountain-Pacific incorporated a virtual component to the pilot. “Nurses have to cover pretty large distances between patients,” says Shadwick, “so we included the use of iPads and video chat to remotely connect nurses to patients as a way to make our work efficient, but still maintain those close relationships between patients and clinicians.”
This technology component is important, but an early finding from the Mountain-Pacific pilot is that the personal relationship that develops between patients and a CHW or volunteer is invaluable to the ReSource Team model. “There’s so much that these teams glean by going into the home that is not shared with medical staff in an office visit,” says Shadwick. “They are able to connect patients to so many services that are outside of the clinic walls and get a better view of the patient’s true living situation.”
Mountain-Pacific in the National Spotlight
The PBS NewsHour — a nightly news broadcast that airs across the United States — recently featured Mountain-Pacific’s innovative efforts to connect rural Montanans to high-quality, cost-effective care, in spite of limited resources and a vastly rural service area. View the video segment.
Lesly Starling, a ReSource Team nurse, says her job is “like putting together the pieces of a puzzle.” She shares the story of one patient, “[a] grandmother living with her son and daughter-in-law. They have the cars during the day when the food bank is open, so she can never get there. She’s got congestive heart failure and is eating Ramen noodles that are high in sodium, because it’s that or nothing.” Without these sort of details, a provider could easily assume that the patient is resistant to changing her diet; in reality, however, she is struggling with unseen obstacles to leading a healthier lifestyle. Fortunately, Lesly and her team were able to link the woman to other food resources within her community.
“There’s so much that these teams glean by going into the home that is not shared with medical staff in an office visit. They are able to connect patients to so many services that are outside of the clinic walls and get a better view of the patient’s true living situation.”
Under the Mountain-Pacific pilot, the ReSource Team’s nurse and a CHW or volunteer first meet with eligible patients when they have been admitted to the hospital. After making this initial connection, they make an appointment to visit the patients in their homes once they have been discharged. At the first in-home meeting, the nurse performs a clinical assessment, including a review of all the medications the patient is taking. During subsequent visits, just the CHW or volunteer returns, bringing along an iPad equipped with a secure video chat function that allows him or her to remotely connect with the ReSource Team nurse, or any other member of the care team.
Clinical concerns, including drug interactions and polypharmacy issues for patients taking four or more medications, can be addressed quickly and from the comfort of the patient’s own home. Nurses also benefit from the video innovation—they can check in on many more patients each week without having to spend hours driving in the car. “Patients can live as far as 30 miles from their health care system,” says Starling. “And that can be 30 miles without anything—cities, stores, a pharmacy.” She adds, “It’s a lot to navigate, especially if you’re not feeling well.”
The Mountain-Pacific pilot also leverages technology to bring ReSource Teams operating in Helena, Billings, and Kalispell together for monthly de-identified patient case conferences and other learning opportunities. There are no intrastate flights that connect those three cities, and Kalispell is eight hours by car from Billings. Conducted by webinar, the video conferences pull in pharmacists, behavioral health consultants, and other experts on a range of topics including care transitions, addiction services, and public or private insurance benefits. “It’s like a brainstorming session that helps keep us all on task and up-to-date,” says Starling. In addition, the ReSource Teams at each site meet with a supervisor once a week in a “ReSource Huddle” to discuss all patients in-depth.
The volunteers in the Mountain-Pacific pilot are primarily older people from the community, including retired loggers, teachers, physical therapists, nurses, and businesspeople. The health care workforce shortages in Montana, as well as a robust volunteer network, made using them an attractive alternative to CHWs in some communities. No previous medical training or experience is required; just an inquisitive mind, and an ability to communicate with people from all walks of life. Sandy Doll, the CHW who assists Starling out in the field, describes the role of volunteers as providing “a different level of caring. They’re paying attention to stuff that nobody else is paying attention to.”
“This field is expanding and we are learning that there’s no one best way to do it. So the more we collaborate, learn from each other and explore, the better for everybody.”
Another innovation to the Montana pilot is the recent addition of veterans to the Billings-based ReSource Team. “One in 10 residents of Montana is a veteran,” says Shadwick, “so more than likely you are going to have a patient, spouse, or family member who has served.” In Billings, the Mountain-Pacific pilot added two veterans as paid CHWs to its care team. Veterans are often better able to make a connection with patients who have served, says Shadwick. “They bring great skills to the program—they have a shared language and experiences, and know how to navigate the Veterans Administration (VA) health system,” a complex system that not all know how to access. In Kalispell, for example, one care team member discovered that a 74-year-old veteran had never signed up for his VA benefits and was covered only by Medicare. As she got to know him better, she learned that the veteran struggled with illiteracy and deciphering his medical bills. After helping him fill out his paperwork to access his VA benefits, the veteran was finally able to afford hearing aids and all of his medication.
ReSource Teams are Driving Results
The Montana TCC pilot is still ramping up, and to date has served 40 patients. Most patients are in their late 50s or older and are suffering from some combination of diabetes, heart disease and chronic obstructive pulmonary disease (COPD). Many also struggle with addiction and/or mental health issues. Although data collection is just beginning, there are clear signs that ReSource Teams are helping these patients better manage their complex medical and social needs. There is also anecdotal evidence that this direct, high-touch approach can lower the cost of caring for the most complex patients.
In Kalispell, for example, Mountain-Pacific referred a woman in her 50s to the ReSource program because her health had declined to the point where she was a candidate for hospice care. When she entered the program, the woman was suffering from multiple conditions including COPD, using an oxygen condenser, and living in her car. In the five months prior to her referral, the hospital had billed Medicare close to $100,000 for her inpatient stays and ED use.
The ReSource Team intervened and helped the woman find affordable housing that would accommodate her beloved dog, provided guidance on managing multiple medications and oxygen, and linked her to a range of other services to support independent living. In the six months after entering the program, hospital charges were below $6,000 as the once-homeless woman had no hospital admissions and only visited the ED two times. And, perhaps most important, she is no longer a candidate for hospice care.
Occasionally, the ReSource Team encounters patients who have been struggling to accept a diagnosis and manage their treatment for years. One such patient was David, a man who had cyclic vomiting syndrome and, according to Starling, “was in the ED every single day, or every other day.” Although extremely mistrustful at first, David was moved that the ReSource Team members cared enough to visit him, and began opening up to them about his financial worries. With time and a lot of paperwork, the ReSource Team successfully managed to keep David from losing his home — a source of anxiety that was negatively affecting his health.
David now adheres to his medication regimen, and “hasn’t been back in the hospital for weeks, maybe even months,” reports Starling. “He did everything we asked him to do. He followed the instructions, and he got better.” She describes the process this way: “Building that relationship with a patient isn’t easy, but once you have that—what you say carries more weight with them. Say they got discharged with instructions on paper…that has a weight of 1, but if you say something to reinforce the instructions? That has a weight of 10.”
Moving Forward
The Mountain-Pacific ReSource Team pilot is designed as a short-term solution. Patients are enrolled for 60-90 days, after which the nurse determines if they are ready to be handed off to their primary care physician. Some patients are ready to transition from the enhanced care management after just 30 days, while others need 90 days or even more to get connected with resources and better manage their health.
Shadwick is optimistic about the ReSource Team model and sees it as being sustainable in Montana and other rural areas. The key is to keep the model evolving and growing and to maintain the collaboration that drives innovation. “This field is expanding and we are learning that there’s no one best way to do it. So the more we collaborate, learn from each other and explore, the better for everybody,” she says.
Author Naomi Freundlich is a journalist with more than 25 years of experience writing about health care.
About the Center for Health Care Strategies
The Center for Health Care Strategies (CHCS) is a nonprofit policy center dedicated to improving the health of low-income Americans. It works with state and federal agencies, health plans, providers, and community-based organizations to develop innovative programs that better serve people with complex and high-cost health care needs. To learn more, visit www.chcs.org.
About Transforming Complex Care
AccessHealth Spartanburg is part of Transforming Complex Care, a multi-site demonstration aimed at refining and spreading effective care models that address the complex medical and social needs of high-need, high-cost patients. This national initiative, made possible with support from the Robert Wood Johnson Foundation and led by CHCS, is working with six organizations to enhance existing complex care programs within a diverse range of delivery system, payment, and geographic environments. For more information, visit www.chcs.org/transforming-complex-care.
*Lara Shadwick is the former regional program director for Mountain-Pacific in Missoula, Montana.




