In discussing Medicaid, we often use jargon, acronyms, and maxims. Pay for value, not volume. Address social determinants of health (SDOH).
Now, we have a new maxim: Pay for Success (PFS). Over the past few years, states and localities have used PFS principles to fund supports for at-risk moms, in-home asthma assessments, and supportive housing. PFS projects typically address SDOH, while maintaining an aggressive focus on outcomes. But until recently, only one state, South Carolina, has used PFS in its Medicaid program.
What Matters: Investing in Results to Build Strong, Vibrant Communities, a recent book published by the Federal Reserve Bank of San Francisco and Nonprofit Finance Fund, discusses the potential impact of PFS on public sector programs. In one chapter, CHCS’ Allison Hamblin outlines how PFS could gain traction in Medicaid. This blog post explores what PFS can bring to Medicaid. It also discusses how PFS can be integrated into Medicaid managed care programs and value-based purchasing (VBP) initiatives, including Medicaid accountable care organization (ACO) programs, and support partnerships with community-based organizations (CBOs).
What is Pay for Success and how can it support Medicaid?
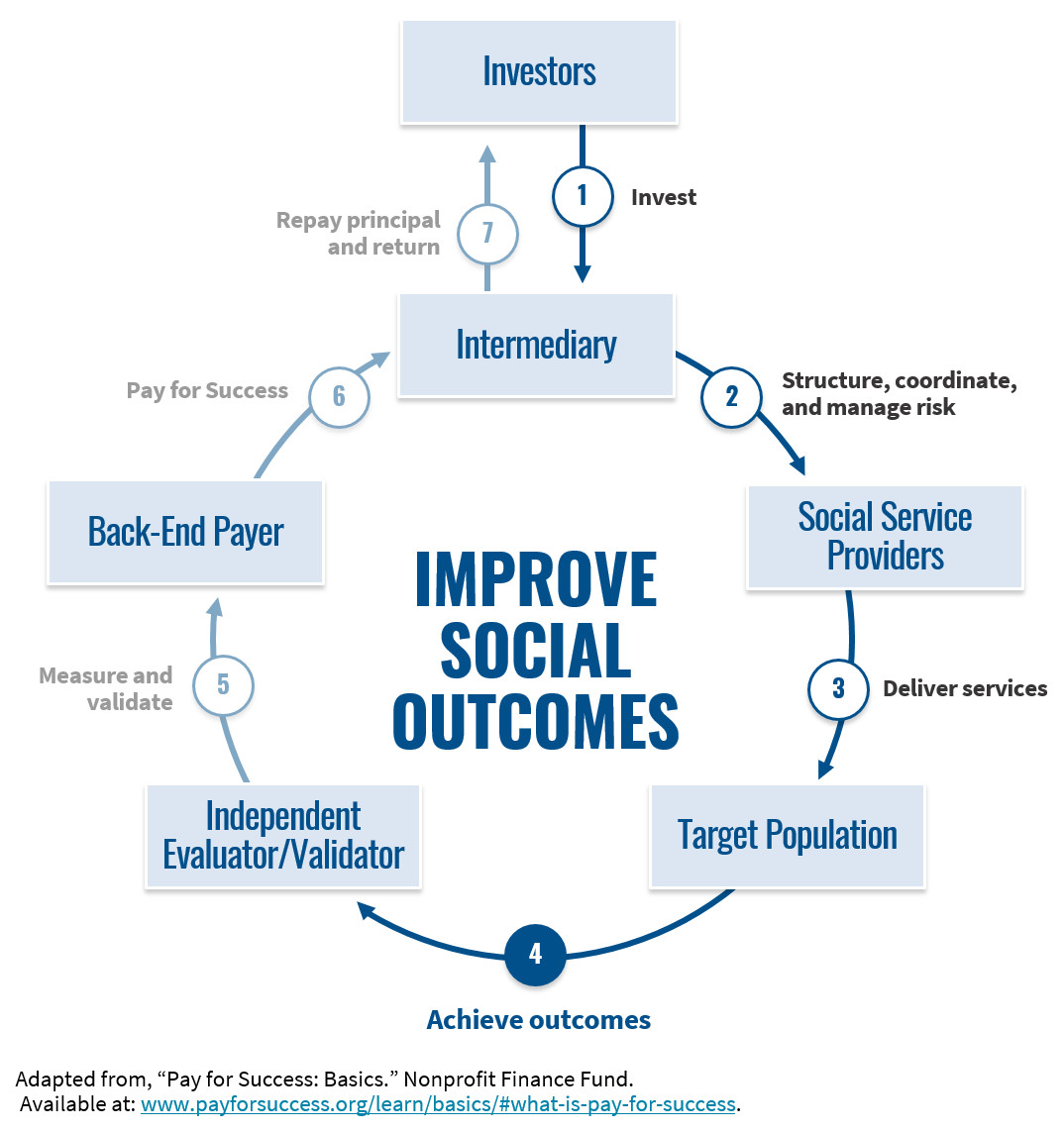
PFS allows entities to contract and pay for outcomes, rather than services. The financial vehicle — the “social impact bond” — typically has two components: (1) an outcomes-based payment; and (2) upfront working capital to cover the costs of service delivery until outcomes are achieved, typically provided by private investors. If the PFS project does not achieve its expected outcomes, no payment is made, and investors are not repaid for their upfront investment.
In many ways, PFS’ principles are consistent with the current momentum of Medicaid policy:
- PFS is a value-based approach. PFS can build upon state VBP initiatives by emphasizing outcomes, instead of focusing on costs.
- PFS encourages investments in SDOH. Health begins where we live, learn, work, and play, and investing in social factors — like housing and family supports — can improve health outcomes.
- PFS scales evidence-based prevention strategies. By facilitating upfront, startup capital for social programs, PFS develops the infrastructure and funding needed for statewide program implementation.
- With PFS, states can define desired outcomes, not new Medicaid service categories. Because of its adaptability to managed care and VBP arrangements, PFS may accelerate the pace with which SDOH interventions are incorporated into Medicaid programs, while maintaining clear boundaries on Medicaid-covered services.
- PFS converts health care funding into more cost-effective social services. As Elizabeth Bradley and her colleagues at Yale University have demonstrated, social service expenditures are significantly associated with better health outcomes.
- PFS identifies new financial resources. PFS gives social programs access to upfront, startup capital that would otherwise not be easily available. And, by attracting private capital and maintaining an aggressive focus on outcomes, PFS could help prepare states to operate in a more resource-constrained environment — where it might be ever more important to only pay for what works.
On the flip side, however, in their current form, PFS transactions are small-scale and fairly complex. They require extensive preparation and negotiation, involve intermediaries and third-party evaluators, and ultimately have impacts on relatively small populations — hundreds of people, rather than the thousands or millions enrolled in state Medicaid programs. Because of these limitations, PFS, in its most traditional form, may be unlikely to achieve broad adoption among state Medicaid agencies.
Nonetheless, PFS could still be an important tool for Medicaid managed care organizations (MCOs) and providers looking to improve health care quality and provide more efficient care. It is an adaptable risk management tool that can help frame complex issues and channel local efforts to address SDOH and improve health outcomes. In addition, emerging PFS approaches — such as the outcomes rate card — can potentially make PFS more scalable and less complex at the state level.
How can Medicaid providers and MCOs use PFS?
Following are two examples that illustrate how PFS could be a useful tool to Medicaid stakeholders by supporting: (1) value-added services provided by an MCO; and (2) community-based organization (CBO) partnerships with providers in VBP arrangements.
Value-Added Services Provided by an MCO
Increasingly, states are looking to their Medicaid MCOs to address members’ SDOH. Notwithstanding that a MCO may not have the expertise to substantially invest in an SDOH intervention, current policies related to covered services and rate-setting also limit MCO incentives to invest in services that fall outside of in-plan benefits. PFS, however, offers a mechanism to improve MCO incentives and reduce the financial risk associated with such investments.
Under 42 C.F.R. § 438.3(e)(1)(i), MCOs may voluntarily provide services beyond those included in the traditional Medicaid benefit package. Although “value-added services” are not considered in the calculation of an MCO’s capitation rates, the cost of value-added services may be included in the numerator of the MCO’s medical loss ratio (MLR), per 42 C.F.R. § 438.8(e)(2)(i)(A).
While an MCO may hesitate to spend funds on services that are not included in its capitation rate, an MCO can use PFS to only pay for services that deliver desired outcomes — including outcomes that may be tied to other performance incentives in their contracts. Furthermore, those expenditures can help the MCO meet its required MLR — 85 percent or higher in some state Medicaid programs.
CBO Partnerships with Providers in VBP Arrangements
As states and MCOs implement VBP and alternative payment models (APM), Medicaid providers are looking for ways to decrease health care expenditures and improve quality. Increasingly, these providers are turning to community partners to help realize the financial incentives in their chosen APM.
In support of their Medicaid ACO and VBP initiatives, some states — like New York, Minnesota, Rhode Island, and Massachusetts — have required or encouraged their Medicaid providers to enter into formal partnerships with CBOs. These policies encourage health care providers to coordinate with organizations that may be better positioned to address SDOH — for example, food and housing insecurity.
PFS arrangements can support these partnerships by allowing Medicaid providers to set up an outcomes-based payment that mirrors the incentivized outcomes in their own APM, while providing CBOs with working capital to cover the upfront cost of service delivery. Instead of just referring patients to CBOs, Medicaid ACOs can use PFS to formalize their partnerships with the CBOs and align their collective quality and cost savings goals. The CBOs, in turn, can offload the risk associated with these outcomes-based contracts to outside investors.
For example, an ACO participating in a shared savings program may define a cost of care benchmark with respect to a particular subset of the population in need of a SDOH intervention. For instance, the Green & Healthy Homes Initiative (GHHI), a provider of home-based asthma interventions, has designed PFS arrangements that reward reductions in the cost of care for children who have had one or more asthma-related visits to the emergency department. Similar to shared savings models, the methodology behind the outcome-based payments is reviewed by an actuary. Adopting this model for an ACO-CBO partnership, PFS investors would provide the CBO with upfront working capital to support home-based asthma interventions. If the asthma program produces desired outcomes, the ACO would pay PFS investors. If the joint asthma effort, among other initiatives, results in savings relative to the ACO’s total cost of care benchmark, a Medicaid MCO or state Medicaid agency would pay the ACO a portion of the savings, in accordance with its VBP arrangement.
What’s Next?
PFS is not a panacea or a replacement for consistent government funding of critical programs. But, PFS concepts can transform how we think about funding for social services and SDOH interventions. We encourage Medicaid stakeholders to think of ways PFS can support their program objectives and to monitor technical assistance opportunities through Social Finance (e.g., Outcomes Rate Card Competition) and GHHI (e.g., Reimbursement Support Request for Proposals). With support from the Robert Wood Johnson Foundation, CHCS may provide technical assistance to states and other Medicaid stakeholders interested in using PFS to further Medicaid policy objectives; if you are interested, contact Diana Crumley at .
Look for a deeper dive into PFS opportunities in an upcoming CHCS blog post: “Outcomes Rate Cards: A Scalable Pay for Success Approach.”




