Value-based payment (VBP) — provider payment models that shift from volume-based fee-for-service (FFS) to support value-driven care delivery — is an important strategy for states seeking to promote innovative primary care approaches through Medicaid managed care. To date, primary care VBP models have been successfully used by states to incentivize quality improvement and support providers in adopting core primary care functions. Significant opportunities to advance primary care VBP still exist, however, largely because most Medicaid VBP is based on FFS reimbursement. As states, payers, and providers gain experience in VBP, they may consider implementing prospective payment models that support practices in offering more comprehensive care, such as through integrating physical and behavioral health care, addressing health-related social needs (HRSNs),and creating opportunities to advance health equity.
Strengthening Primary Care through Medicaid Managed Care

This blog post is part of a learning series from the Center for Health Care Strategies, Strengthening Primary Care through Medicaid Managed Care. The ongoing series is examining the tools that states can use to advance comprehensive primary care strategies and equitably improve the health of Medicaid enrollees. This series of webinars, resources, and blog posts is made possible by The Commonwealth Fund.
Prospective Payment as a Lever to Support High-Quality Primary Care
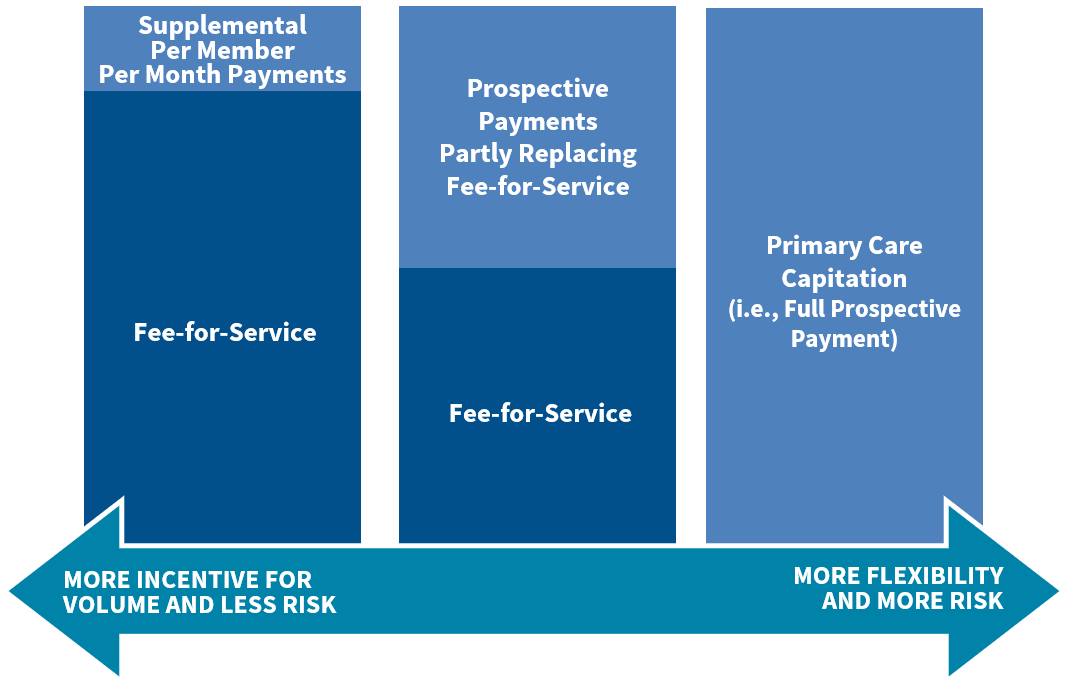
FFS payment incentivizes a high volume of short visits for health care services and often does not reimburse, or inadequately reimburses, primary care providers for high-value services. Implementing VBP that relies more on prospective payments — upfront payments not tied to specific service codes — may allow providers more flexibility and the financial stability needed to implement innovative primary care delivery models. There are a range of ways payers can implement prospective payments, depending on the capacity of providers to take on financial risk and manage population health. For providers with less VBP experience, payers may consider implementing prospective payment mechanisms alongside FFS to build capacity and enable a gradual transition to fully prospective payment models. Following are steps that states can take to move along the continuum from volume-based, FFS payment to value-based, prospective payment with more flexibility to pay for services as needed.
Progressing Toward Prospective Payment in Primary Care
- Introduce Supplemental Per Member Per Month Payments. To begin the transition to prospective payment, states may consider providing supplemental per member per month payment, on top of FFS, to support enhanced primary care capabilities. For example, states such as Tennessee and Ohio have used participation in the Comprehensive Primary Care Plus (CPC+) program to implement such models.
- Partly Replace FFS with Prospective Payments. States can also bridge the transition between FFS and full prospective payment using hybrid capitated models in which prospective payment only partially replaces FFS payment. For example, the Center for Medicare and Medicaid Innovation’s Primary Care First model includes both a prospective Population-Based Payment, a Flat Primary Care Visit Fee, and a quality-based performance adjustment.
- Fully Transition to Primary Care Capitation. Primary care providers with experience in risk-based VBP may be ready to participate in fully capitated models in which providers are paid upfront for a broad array of services. Capitated models provide significantly more flexibility than FFS, but also an increased level of financial risk. For instance, Washington State is working to implement a multi-payer primary care VBP model that uses a prospective Comprehensive Primary Care Payment to cover a broad array of services. This payment will be supplemented by a Transformation of Care Fee which will transition over time into a performance-based payment.
Tying Prospective Payment to Primary Care Delivery Goals
Prospective payments can be a particularly powerful tool to support advanced primary care when paired with explicit incentives and design elements that support states’ primary care delivery goals, such as the ones below. The flexibility of prospective payment can allow providers the ability to offer services or care models that support state goals, and quality measures can be used to reinforce these efforts.
- Advance health equity. Health disparities can be mitigated through access to high quality primary care, highlighting the opportunity for primary care VBP to serve as a lever for advancing health equity. Developing equity-focused primary care VBP models requires engaging patients and other stakeholders to define equity goals and intentionally design payment elements to achieve these aims. To identify disparities and stratify quality measures, states should consider how to support or incentivize improved race, ethnicity, and language data collection among providers — with the ultimate goal of tying prospective payment to health disparity reductions in primary care. It is also important to consider and avoid unintended consequences of VBP efforts, such as penalizing providers who care for populations with complex needs, which can exacerbate disparities.
- Integrate behavioral health care into primary care. There is an extensive evidence base that integrating behavioral health care — including care for substance use disorders and mental illness — into primary care can improve health outcomes. Integration may include a continuum of interventions, ranging from behavioral health screening and referrals to fully integrated physical and behavioral health care within a care setting. States may consider defining the model or level of integration they aim to achieve through prospective payment. For example, the Center for Medicare and Medicaid Innovation’s CPC+ model provides increased payment to primary care practices to support enhanced primary care functions, including behavioral health integration. States, like Ohio, Tennessee, and New York, are also adopting or recommending behavioral health quality measures as part of primary care VBP models, including for depression, substance use disorder, and other conditions.
- Address health-related social needs. Primary care’s role as the first touchpoint for patients with the health care system and the locus of care coordination provides significant opportunity for practices to identify and address HRSNs. Because effectively addressing HRSNs requires cross-sector collaboration, states implementing prospective payment may consider defining expectations for primary care providers’ role. For example, the Ohio Comprehensive Primary Care program requires practices to demonstrate a process for identifying social needs and connecting patients to community resources in order to qualify for enhanced payment. Additionally, strategies such as implementing risk-adjustment methodologies that account for social risk factors, as Massachusetts’ and Minnesota’s accountable care organization programs have done, have the potential to provide more resources to providers caring for populations with complex needs. States may also consider whether additional infrastructure investments are needed to support collaboration and data sharing between primary care and other sectors, especially for smaller practices. For example, North Carolina and Pennsylvania are investing in community referral platforms to offer a common tool for primary care and other providers. Finally, while quality measurement approaches related to HRSNs are relatively nascent, some states like Massachusetts and Rhode Island have implemented HRSN screening measures as part of their accountable care organization programs.
Opportunities to Learn More
Prospective payment models that offer primary care practices increased flexibility for innovation in care, while holding them accountable for quality, can support states in achieving their primary care goals. These themes were further explored in a recent CHCS webinar, Implementing Primary Care Value-Based Payment through Medicaid Managed Care. Additional considerations for developing primary care VBP in Medicaid managed care can be found in the Move to Value-Based Payment in Primary Care module of CHCS’ Advancing Primary Care Innovation in Medicaid Managed Care toolkit.